Abstract
Introduction and hypothesis
We compared pelvic organ prolapse (POP) repair with and without midurethral sling (MUS) in women with occult stress urinary incontinence (SUI).
Methods
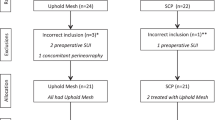
This was a randomized trial conducted by a consortium of 13 teaching hospitals assessing a parallel cohort of continent women with symptomatic stage II or greater POP. Women with occult SUI were randomly assigned to vaginal prolapse repair with or without MUS. Women without occult SUI received POP surgery. Main outcomes were the absence of SUI at the 12-month follow-up based on the Urogenital Distress Inventory and the need for additional treatment for SUI.
Results
We evaluated 231 women, of whom 91 randomized as follows: 43 to POP surgery with and 47 without MUS. A greater number of women in the MUS group reported absence of SUI [86 % vs. 48 %; relative risk (RR) 1.79; 95 % confidence interval (CI) 1.29–2.48]. No women in the MUS group received additional treatment for postoperative SUI; six (13 %) in the control group had a secondary MUS. Women with occult SUI reported more urinary symptoms after POP surgery and more often underwent treatment for postoperative SUI than women without occult SUI.
Conclusions
Women with occult SUI had a higher risk of reporting SUI after POP surgery compared with women without occult SUI. Adding a MUS to POP surgery reduced the risk of postoperative SUI and the need for its treatment in women with occult SUI. Of women with occult SUI undergoing POP-only surgery, 13 % needed additional MUS. We found no differences in global impression of improvement and quality of life.

Similar content being viewed by others
References
Lensen EJM, Withagen MIJ, Kluivers KB, Milani AL, Vierhout ME (2013) Urinary incontinence after surgery for pelvic organ prolapse. Neurourol Urodyn 32(5):455
Brubaker L, Cundiff GW, Fine P, Nygaard I, Richter HE, Visco AG et al (2006) Abdominal sacrocolpopexy with Burch colposuspension to reduce urinary stress incontinence. N Engl J Med 354(15):1557–1566
Wei JT, Nygaard I, Richter HE, Nager CW, Barber MD, Kenton K et al (2012) A midurethral sling to reduce incontinence after vaginal prolapse repair. N Engl J Med 366(25):2358–2367
van der Ploeg J, van der Steen A, Oude Rengerink K, van der Vaart C, Roovers J (2014) Prolapse surgery with or without stress incontinence surgery for pelvic organ prolapse: a systematic review and meta-analysis of randomised trials. BJOG 121(5):537–547
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J Pelvic Floor Dysfunct 21(1):5–26
Hafidh BA, Chou Q, Khalil MM, Al-Mandeel H (2013) De novo stress urinary incontinence after vaginal repair for pelvic organ prolapse: one-year follow-up. Eur J Obstet Gynecol Reprod Biol
Jundt K, Wagner S, von Bodungen V, Friese K, Peschers UM (2010) Occult incontinence in women with pelvic organ prolapse - Does it matter? Eur J Med Res 15(3):112–116
Araki I, Haneda Y, Mikami Y, Takeda M (2009) Incontinence and detrusor dysfunction associated with pelvic organ prolapse: clinical value of preoperative urodynamic evaluation. Int Urogynecol J Pelvic Floor Dysfunct 20(11):1301–1306
Svenningsen R, Borstad E, Spydslaug AE, Sandvik L, Staff AC (2012) Occult incontinence as predictor for postoperative stress urinary incontinence following pelvic organ prolapse surgery. Int Urogynecol J 23(7):843–849
Fuentes A (2011) A prospective randomised controlled trial comparing vaginal prolapse repair with and without tensionfree vaginal tape transobturator tape (TVTO) in women with severe genital prolapse and occult stress incontinence: long term follow up. Int Urogynecol J Pelvic Floor Dysfunct 22(S1):S60
Schierlitz L, Dwyer PL, Rosamilia A, De Souza A, Murray C, Thomas E et al (2014) Pelvic organ prolapse surgery with and without tension-free vaginal tape in women with occult or asymptomatic urodynamic stress incontinence: a randomised controlled trial. Int Urogynecol J 25(1):33–40
Ennemoser S, Schonfeld M, von Bodungen V, Dian D, Friese K, Jundt K (2012) Clinical relevance of occult stress urinary incontinence (OSUI) following vaginal prolapse surgery: long-term follow-up. Int Urogynecol J 23(7):851–855
Khoshbakht N, Alarab M, Lovatsis D (2012) Stress urinary incontinence six months post laparoscopic sacrocolpopexy. J Obstet Gynaecol Can 34(7):653–656
Khelaia V, Khelaia V (2010) Anti-incontinence procedures in women with severe urogenital prolapse. Eur Urol Suppl 9(6):565
Kasturi S, Diaz SI, McDermott CD, Woodman PJ, Bump RC, Terry CL et al (2011) De novo stress urinary incontinence after negative prolapse reduction stress testing for total vaginal mesh procedures: incidence and risk factors. Am J Obstet Gynecol 205(5):487.e1–487.e4
Liapis A, Bakas P, Georgantopoulou C, Creatsas G (2011) The use of the pessary test in preoperative assessment of women with severe genital prolapse. Eur J Obstet Gynecol Reprod Biol 155(1):110–113
van der Ploeg J, Oude Rengerink K, van der Steen A, van Leeuwen J, Stekelenburg J, Bongers M, et al. (2015) Transvaginal prolapse repair with or without the addition of a midurethral sling in women with genital prolapse and stress urinary incontinence: a randomised trial. BJOG
van der Steen A, van der Ploeg M, Dijkgraaf MG, van der Vaart H, Roovers JP (2010) Protocol for the CUPIDO trials; multicenter randomized controlled trials to assess the value of combining prolapse surgery and incontinence surgery in patients with genital prolapse and evident stress incontinence (CUPIDO I) and in patients with genital prolapse and occult stress incontinence (CUPIDO II). BMC Womens Health 10:16
Visco AG, Brubaker L, Nygaard I, Richter HE, Cundiff G, Fine P et al (2008) The role of preoperative urodynamic testing in stress-continent women undergoing sacrocolpopexy: the Colpopexy and Urinary Reduction Efforts (CARE) randomized surgical trial. Int Urogynecol J Pelvic Floor Dysfunct 19(5):607–614
van der Vaart CH, de Leeuw JRJ, Roovers JWR, Heintz APM (2003) Measuring health-related quality of life in women with urogenital dysfunction: the urogenital distress inventory and incontinence impact questionnaire revisited. Neurourol Urodyn 22(2):97–104
Mitropoulos D, Artibani W, Graefen M, Remzi M, Rouprêt M, Truss M (2012) Reporting and grading of complications after urologic surgical procedures: an ad hoc EAU guidelines panel assessment and recommendations. Eur Urol 61(2):341–349
Strasberg SM, Linehan DC, Hawkins WG (2009) The accordion severity grading system of surgical complications. Ann Surg 250(2):177–186
Parker-Autry CY, Barber MD, Kenton K, Richter HE (2013) Measuring outcomes in urogynecological surgery: “perspective is everything”. Int Urogynecol J 24(1):15–25
Haessler AL, Lin LL, Ho MH, Betson LH, Bhatia NN (2005) Reevaluating occult incontinence. Curr Opin Obstet Gynecol 17(5):535–540
Cohen J (ed) (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawence Earlbaum Associates, Hillsdale
Costantini E, Lazzeri M, Bini V, Del Zingaro M, Zucchi A, Porena M (2011) Pelvic organ prolapse repair with and without prophylactic concomitant burch colposuspension in continent women: a randomized, controlled trial with 8-year follow up. J Urol 185(6):2236–2240
Brubaker L, Nygaard I, Richter HE, Visco A, Weber AM, Cundiff GW et al (2008) Two-year outcomes after sacrocolpopexy with and without burch to prevent stress urinary incontinence. Obstet Gynecol 112(1):49–55
Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4:CD004014
Borstad E, Abdelnoor M, Staff AC, Kulseng-Hanssen S (2010) Surgical strategies for women with pelvic organ prolapse and urinary stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 21(2):179–186
Stekkinger E, van der Linden PJ (2011) A comparison of suprapubic and transurethral catheterization on postoperative urinary retention after vaginal prolapse repair: a randomized controlled trial. Gynecol Obstet Investig 72(2):109–116
Hakvoort RA, Dijkgraaf MG, Burger MP, Emanuel MH, Roovers JP (2009) Predicting short-term urinary retention after vaginal prolapse surgery. Neurourol Urodyn 28(3):225–228
Jelovsek JE, Chagin K, Brubaker L, Rogers RG, Richter HE, Arya L et al (2014) A model for predicting the risk of de novo stress urinary incontinence in women undergoing pelvic organ prolapse surgery. Obstet Gynecol 123(2 Pt 1):279–287
Lo TS, Bt Karim N, Nawawi EA, Wu PY, Nusee Z (2015) Predictors for de novo stress urinary incontinence following extensive pelvic reconstructive surgery. Int Urogynecol J
Acknowledgments
We thank the Dutch Urogynecology Consortium for data collection: Marlies Y. Bongers, Karin S. Dekker, Hugo W.F. van Eijndhoven, Iris van Gestel, Kirsten B. Kluivers, Gerold Link, Aaltje J. Schram (deceased), Jelle Stekelenburg, Annemarie E. Weis-Potters and Jac Wijma.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
An unrestricted grant was received by the Dutch Ohra Fund.
Conflicts of interest
Jan-Paul W.R. Roovers: medical consultant for American Medical Systems (AMS). C. Huub van der Vaart: medical consultant for consultancy for BARD Medical.
Ethical approval
The study was conducted in accordance with ethical principles derived from the Declaration of Helsinki, Good Clinical Practice, and International Conference of Harmonization Guidelines. All patients provided written informed consent. Ethical approval was provided by the institutional review board of the Academic Medical Centre in Amsterdam (MEC 05/286, January 2006), and all boards of the participating hospitals.
Additional information
The complete list of authors and collaborators from the Dutch Urogynaecology Consortium are listed in Supporting Information, Table A1 of the “Appendix”.
Trial registration
The Netherlands Trial Register NTR1070 (www.trialregister.nl).
Study website
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 322 kb)
Rights and permissions
About this article
Cite this article
van der Ploeg, J.M., Rengerink, K.O., van der Steen, A. et al. Vaginal prolapse repair with or without a midurethral sling in women with genital prolapse and occult stress urinary incontinence: a randomized trial. Int Urogynecol J 27, 1029–1038 (2016). https://doi.org/10.1007/s00192-015-2924-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2924-1