Abstract
Introduction and hypothesis
Gellhorn and shelf pessaries can be effective management for women with pelvic organ prolapse (POP). This study aimed to investigate the opinion of IUGA members about shelf/Gellhorn pessary use, and in particular, how often to change them in patients with POP. There are no evidence-based guidelines available on this subject.
Methods
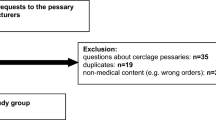
Members of the International Urogynaecology Association (IUGA) and the British Society of Urogynaecology (BSUG) were sent a single electronic mailing of semi-structured questionnaires containing closed and open questions and free text response boxes. The internet-based survey consisted of 13 questions. Free text responses were analysed using a thematic qualitative analysis.
Results
A total of 322 respondents from the IUGA membership participated in the survey. Most consider shelf/Gellhorn pessaries an effective first-line treatment for their patients with POP. Self care is usually acceptable with ring pessaries, but with shelf/Gellhorn, 35 % would like to change them every 3 months, 31 % every 6 months and the rest varied. The routine use of oestrogens along with shelf/Gellhorn pessaries is a common practice. The risk of urogenital fistulae is well documented, but overall clinicians felt that shelf/Gellhorn pessaries are a safe and effective treatment for POP.
Conclusions
This study highlights the wide variation in global practice of the management of shelf/Gellhorn pessaries for POP. In order to inform our practice, evidence-based guidelines are required. A randomised control trial may help to decide whether or not it is appropriate to change the shelf/Gellhorn pessaries at all.
Similar content being viewed by others
References
Cardozo L, Staskin D (2002) Textbook of female urology and urogynaecology. Martin Dunitz, London
Abdool Z, Thakar R, Sultan AH (2011) Prospective evaluation of outcome of vaginal pessaries versus surgery in women with symptomatic pelvic organ prolapse. Int Urogynecol J 22:273–278
Adams E, Thomson A, Maher C, Hagen S (2004) Mechanical devices for pelvic organ prolapse in women. Cochrane Database Syst Rev(2) : CD004010. doi:10.1002/14651858
Lamers BH, Broekman BM, Milani AL (2011) Pessary treatment for pelvic organ prolapse and health-related quality of life: a review. Int Urogynecol J 22:637–644
Gorti M, Hudelist G, Simons A (2009) Evaluation of vaginal pessary management: a UK-based survey. J Obstet Gynaecol 29(2):129–131
Edwards PJ, Roberts I, Clarke MJ, DiGuiseppi C, Wentz R, Kwan I et al. (2009) Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev (3):MR000008. doi:10.1002/14651858.MR000008.pub4
Jones K, Harmanli O (2010) Pessary use in pelvic organ prolapse and urinary incontinence. Rev Obstet Gynecol 3(1):3–9
Russel JK (1961) The dangerous pessary. BMJ 2:1595–1597
Sivasuriya M (1987) Cervical entrapment of a polyethylene vaginal ring pessary—a clinical curiosity. Aust N Z J Obstet Gynaecol 27:168–169
Mueller-Heubach E (1970) A pessary can be dangerous. J Med Soc NJ 67:104–106
Summer J, Ford ML (1971) The forgotten pessary: a medical oddity. Am J Obstet Gynecol 15:1048–1051
Poma PA (1981) Management of incarcerated vaginal pessaries. J Am Geriatr Soc 29:325–327
Goldstein I, Wise GJ, Tancer ML (1990) A vesicovaginal fistula and intravesical foreign body: a rare case of the neglected pessary. Am J Obstet Gynecol 163(2):589–591
Roberge RJ, McCandlish MM, Dorfsman ML (1999) Urosepsis associated with vaginal pessary use. Ann Emerg Med 33:581–583
Ott R, Richter H, Behr J, Scheele J (1993) Small bowel prolapse incarceration caused by a vaginal ring pessary. Br J Surg 80:1157
Arias BE, Ridgeway B, Barber MD (2008) Complications of neglected vaginal pessaries: case presentation and literature review. Int Urogynecol J Pelvic Floor Dysfunct 19(8):1173–1178
Schraub S, Sun XS, Maingon P et al (1992) Cervical and vaginal cancer associated with pessary use. Cancer 69:2505–2509
Oliver R, Thakar R, Sultan AHÔ (2011) The history and use of vaginal pessary: a review. Eur J Obstet Gynaecol Reprod Biol 156:125–130
Pott-Grinstein E, Newcomer JR (2001) Gynaecologists’ pattern of prescribing pessaries. J Reprod Med 46:205–208
Cundiff WG, Weidner AC, Visco AG, Bump RC, Addison A (2000) A survey of pessary use by members of the American Urogynaecologic Society. Obstet Gynaecol 95(6 Pt 1):931–935
Bugge C, Hagen S, Thakar R (2013) Vaginal pessaries for pelvic organ prolapse and urinary incontinence: a multi-professional survey of practice. Int Urogynecol J 24:1017–1024
Storey S, Aston M, Price S, Irving L, Hemmens E (2009) Women’s experiences with vaginal pessary use. J Adv Nurs 65(11):2350–2357
Haslam J (2004) Nursing management of stress urinary incontinence in women. Br J Nurs 13(1):32–40
Acknowledgement
We acknowledge the contribution of those who responded to the questionnaire.
Conflicts of interest
AK: none; RMF: partially supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula. The views expressed in this publication are those of the author and not necessarily those of the NHS, the NIHR or the Department of Health.
Disclosures
RMF has received speaker fees for educational lectures for meetings sponsored by Astellas and Pfizer; author on standardisation reports; scientific editor for IUJ; Vice-President IUGA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khaja, A., Freeman, R.M. How often should shelf/Gellhorn pessaries be changed? A survey of IUGA urogynaecologists. Int Urogynecol J 25, 941–946 (2014). https://doi.org/10.1007/s00192-014-2329-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2329-6