Abstract
Purpose
Hyperlactatemia may occur for a variety of reasons and is a predictor of poor clinical outcome. However, only limited data are available on the underlying causes of hyperlactatemia and the mortality rates associated with severe hyperlactatemia in critically ill patients. We therefore aimed to evaluate the etiology of severe hyperlactatemia (defined as a lactate level >10 mmol/L) in a large cohort of unselected ICU patients. We also aimed to evaluate the association between severe hyperlactatemia and lactate clearance with ICU mortality.
Methods
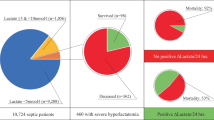
In this retrospective, observational study at an University hospital department with 11 ICUs during the study period between 1 April 2011 and 28 February 2013, we screened 14,040 ICU patients for severe hyperlactatemia (lactate >10 mmol/L).
Results
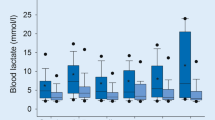
Overall mortality in the 14,040 ICU patients was 9.8 %. Of these, 400 patients had severe hyperlactatemia and ICU mortality in this group was 78.2 %. Hyperlactatemia was associated with death in the ICU [odds ratio 1.35 (95 % CI 1.23; 1.49; p < 0.001)]. The main etiology for severe hyperlactatemia was sepsis (34.0 %), followed by cardiogenic shock (19.3 %), and cardiopulmonary resuscitation (13.8 %). Patients developing severe hyperlactatemia >24 h of ICU treatment had a significantly higher ICU mortality (89.1 %, 155 of 174 patients) than patients developing severe hyperlactatemia ≤24 h of ICU treatment (69.9 %, 158 of 226 patients; p < 0.0001). Lactate clearance after 12 h showed a receiver-operating-characteristics area under the curve (ROC-AUC) value of 0.91 to predict ICU mortality (cut-off showing highest sensitivity and specifity was a 12 h lactate clearance of 32.8 %, Youden Index 0.72). In 268 patients having a 12-h lactate clearance <32.8 % ICU mortality was 96.6 %.
Conclusions
Severe hyperlactatemia (>10 mmol/L) is associated with extremely high ICU mortality especially when there is no marked lactate clearance within 12 h. In such situations, the benefit of continued ICU therapy should be evaluated.





Similar content being viewed by others
References
Doherty JR, Cleveland JL (2013) Targeting lactate metabolism for cancer therapeutics. J Clin Investig 123:3685–3692
Kraut JA, Madias NE (2014) Lactic acidosis. N Engl J Med 371:2309–2319
Saugel B, Trepte CJ, Heckel K, Wagner JY, Reuter DA (2015) Hemodynamic management of septic shock: is it time for ‘individual goal-directed hemodynamic therapy’ and for specifically targeting the microcirculation? Shock 43:522–529
Ince C (2005) The microcirculation is the motor of sepsis. Crit Care 9(Suppl 4):S13–S19
Vincent JL, De Backer D (2005) Microvascular dysfunction as a cause of organ dysfunction in severe sepsis. Crit Care 9(Suppl 4):S9–S12
Vincent JL, De Backer D (2013) Circulatory shock. N Engl J Med 369:1726–1734
Barth E, Albuszies G, Baumgart K, Matejovic M, Wachter U, Vogt J, Radermacher P, Calzia E (2007) Glucose metabolism and catecholamines. Crit Care Med 35:S508–S518
Cady LD Jr, Weil MH, Afifi AA, Michaels SF, Liu VY, Shubin H (1973) Quantitation of severity of critical illness with special reference to blood lactate. Crit Care Med 1:75–80
Kaplan LJ, Kellum JA (2004) Initial pH, base deficit, lactate, anion gap, strong ion difference, and strong ion gap predict outcome from major vascular injury. Crit Care Med 32:1120–1124
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL, Vincent JL, Rhodes A (2014) Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of intensive care medicine. Intensive Care Med 40:1795–1815
Falk JL, Rackow EC, Leavy J, Astiz ME, Weil MH (1985) Delayed lactate clearance in patients surviving circulatory shock. Acute Care 11:212–215
Vincent JL, Dufaye P, Berre J, Leeman M, Degaute JP, Kahn RJ (1983) Serial lactate determinations during circulatory shock. Crit Care Med 11:449–451
Marik PE, Bellomo R (2015) Lactate clearance as a target of therapy in sepsis: a flawed paradigm. OA Crit Care 01(1):3
Gu WJ, Zhang Z, Bakker J (2015) Early lactate clearance-guided therapy in patients with sepsis: a meta-analysis with trial sequential analysis of randomized controlled trials. Intensive Care Med 41:1862–1863
Gunnerson KJ, Saul M, He S, Kellum JA (2006) Lactate versus non-lactate metabolic acidosis: a retrospective outcome evaluation of critically ill patients. Crit Care 10:R22
Nichol AD, Egi M, Pettila V, Bellomo R, French C, Hart G, Davies A, Stachowski E, Reade MC, Bailey M, Cooper DJ (2010) Relative hyperlactatemia and hospital mortality in critically ill patients: a retrospective multi-centre study. Crit Care 14:R25
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Bakker J, Coffernils M, Leon M, Gris P, Vincent JL (1991) Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock. Chest 99:956–962
Bernardin G, Pradier C, Tiger F, Deloffre P, Mattei M (1996) Blood pressure and arterial lactate level are early indicators of short-term survival in human septic shock. Intensive Care Med 22:17–25
Marecaux G, Pinsky MR, Dupont E, Kahn RJ, Vincent JL (1996) Blood lactate levels are better prognostic indicators than TNF and IL-6 levels in patients with septic shock. Intensive Care Med 22:404–408
Moomey CB Jr, Melton SM, Croce MA, Fabian TC, Proctor KG (1999) Prognostic value of blood lactate, base deficit, and oxygen-derived variables in an LD50 model of penetrating trauma. Crit Care Med 27:154–161
Schreiber J, Nierhaus A, Vettorazzi E, Braune SA, Frings DP, Vashist Y, Izbicki JR, Kluge S (2014) Rescue bedside laparotomy in the intensive care unit in patients too unstable for transport to the operating room. Crit Care 18:R123
Khosravani H, Shahpori R, Stelfox HT, Kirkpatrick AW, Laupland KB (2009) Occurrence and adverse effect on outcome of hyperlactatemia in the critically ill. Crit Care 13:R90
Bakker J, Jansen TC (2007) Dont take vitals, take a lactate. Intensive Care Med 33:1863–1865
Varpula M, Tallgren M, Saukkonen K, Voipio-Pulkki LM, Pettila V (2005) Hemodynamic variables related to outcome in septic shock. Intensive Care Med 31:1066–1071
Maillet JM, Le Besnerais P, Cantoni M, Nataf P, Ruffenach A, Lessana A, Brodaty D (2003) Frequency, risk factors, and outcome of hyperlactatemia after cardiac surgery. Chest 123:1361–1366
Martin MJ, FitzSullivan E, Salim A, Brown CV, Demetriades D, Long W (2006) Discordance between lactate and base deficit in the surgical intensive care unit: which one do you trust? Am J Surg 191:625–630
Broder G, Weil MH (1964) Excess lactate: an index of reversibility of shock in human patients. Science 143:1457–1459
Juneja D, Singh O, Dang R (2011) Admission hyperlactatemia: causes, incidence, and impact on outcome of patients admitted in a general medical intensive care unit. J Crit Care 26:316–320
Casserly B, Phillips GS, Schorr C, Dellinger RP, Townsend SR, Osborn TM, Reinhart K, Selvakumar N, Levy MM (2015) Lactate measurements in sepsis-induced tissue hypoperfusion: results from the surviving sepsis campaign database. Crit Care Med 43:567–573
Leone M, Bechis C, Baumstarck K, Ouattara A, Collange O, Augustin P, Annane D, Arbelot C, Asehnoune K, Baldesi O, Bourcier S, Delapierre L, Demory D, Hengy B, Ichai C, Kipnis E, Brasdefer E, Lasocki S, Legrand M, Mimoz O, Rimmele T, Aliane J, Bertrand PM, Bruder N, Klasen F, Friou E, Levy B, Martinez O, Peytel E, Piton A, Richter E, Toufik K, Vogler MC, Wallet F, Boufi M, Allaouchiche B, Constantin JM, Martin C, Jaber S, Lefrant JY (2015) Outcome of acute mesenteric ischemia in the intensive care unit: a retrospective, multicenter study of 780 cases. Intensive Care Med 41(4):667–676
Bakker J, Gris P, Coffernils M, Kahn RJ, Vincent JL (1996) Serial blood lactate levels can predict the development of multiple organ failure following septic shock. Am J Surg 171:221–226
Jansen TC, van Bommel J, Mulder PG, Lima AP, van der Hoven B, Rommes JH, Snellen FT, Bakker J (2009) Prognostic value of blood lactate levels: does the clinical diagnosis at admission matter? J Trauma 66:377–385
Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA, Tomlanovich MC (2004) Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med 32:1637–1642
Hajjar LA, Almeida JP, Fukushima JT, Rhodes A, Vincent JL, Osawa EA, Galas FR (2013) High lactate levels are predictors of major complications after cardiac surgery. J Thorac Cardiovasc Surgery 146:455–460
Kogan A, Preisman S, Bar A, Sternik L, Lavee J, Malachy A, Spiegelstein D, Berkenstadt H, Raanani E (2012) The impact of hyperlactatemia on postoperative outcome after adult cardiac surgery. J Anesth 26:174–178
O’Connor ED, Fraser JF (2010) Hyperlactatemia in critical illness and cardiac surgery. Crit Care 14:421
Cheung PY, Finer NN (1994) Plasma lactate concentration as a predictor of death in neonates with severe hypoxemia requiring extracorporeal membrane oxygenation. J Pediatr 125:763–768
Sviri S, van Heerden PV (2014) Discussing end-of-life decisions in the ICU-are we doing our best? Crit Care Med 42:1560–1561
Luce JM (2010) End-of-life decision making in the intensive care unit. Am J Respir Crit Care Med 182:6–11
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
MP is a member of the Medical Advisory Board of Radiometer Medical. All other authors declare no conflict of interest.
Source of funding
The complete study was funded internally by the Center of Anesthesiology and Intensive Care Medicine of the University Medical Center Hamburg-Eppendorf.
Additional information
Take-home message: Severe hyperlactatemia (>10 mmol/l) was associated with very high mortality, especially in patients requiring extracorporeal organ support or when severe hyperlactatemia persisted for long periods. Patients’ chances of survival were substantially increased when severe hyperlactatemia was attributed to reversible pathophysiology such as cardiac surgery or seizure; therefore, the etiology of severe hyperlactatemia should be clearly defined in ICU patients if it is used to evaluate prognosis or as a basis for decisions about continuing ICU therapy.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Haas, S.A., Lange, T., Saugel, B. et al. Severe hyperlactatemia, lactate clearance and mortality in unselected critically ill patients. Intensive Care Med 42, 202–210 (2016). https://doi.org/10.1007/s00134-015-4127-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-4127-0