Abstract
Purpose
The decision to start venovenous extracorporeal membrane oxygenation (VV ECMO) is commonly based on the severity of respiratory failure, with little consideration of the extrapulmonary organ function. The aim of the study was to identify predictors of mortality and to develop a score allowing a better stratification of patients at the time of VV ECMO initiation.
Methods
This was a prospective multicenter cohort study on 60 patients with influenza A (H1N1)-associated respiratory distress syndrome participating in the Italian ECMOnet data set in the 2009 pandemic. Criteria for ECMO institution were standardized according to national guidelines.
Results
The survival rate in patients treated with ECMO was 68 %. Significant predictors of death before ECMO institution by multivariate analysis were hospital length of stay before ECMO institution (OR = 1.52, 95 % CI 1.12–2.07, p = 0.008); bilirubin (OR = 2.32, 95 % CI 1.52–3.52, p < 0.001), creatinine (OR = 7.38, 95 % CI 1.43–38.11, p = 0.02) and hematocrit values (OR = 0.82, 95 % CI 0.72–0.94, p = 0.006); and mean arterial pressure (OR = 0.92, 95 % CI 0.88–0.97, p < 0.001). The ECMOnet score was developed based on these variables, with a score of 4.5 being the most appropriate cutoff for mortality risk prediction. The high accuracy of the ECMOnet score was further confirmed by ROC analysis (c = 0.857, 95 % CI 0.754–0.959, p < 0.001) and by an independent external validation analysis (c = 0.694, 95 % CI 0.562–0.826, p = 0.004).
Conclusions
Mortality risk for patients receiving VV ECMO is correlated to the extrapulmonary organ function at the time of ECMO initiation. The ECMOnet score is a tool for the evaluation of the appropriateness and timing of VV ECMO in acute lung failure.
Similar content being viewed by others
Introduction
Extracorporeal membrane oxygenation (ECMO) is a valuable therapeutic option for patients with acute lung failure [1]. During the 2009 H1N1 influenza A pandemic, the use of venovenous (VV) ECMO represented a successful rescue treatment for acute respiratory distress syndrome (ARDS) in patients failing conventional ventilation techniques [2]. Due to its additional costs and the need for trained expertise, however, a rational allocation of this limited resource is of fundamental importance.
Referral and transfer of patients with H1N1-related ARDS to specialized ECMO centers have been shown to be associated with a lower risk of death compared to non-ECMO-referred patients [3].
Currently, the decision to start ECMO is based on commonly used pulmonary scores assessing the severity of respiratory failure, such as Murray’s acute lung injury score and the oxygenation index. A Murray score >3 was used for enrollment and randomization in the “Conventional ventilation versus ECMO for Severe Adult Respiratory failure” (CESAR) Trial [1], as it identifies severely hypoxemic patients failing protective mechanical ventilation with an estimated mortality risk higher than 50 % in comparison to conventional treatment.
Oxygenation failure, however, is rarely the direct cause of death in ECMO patients. On the contrary, a poor outcome is more likely to be determined by the presence of complications [4]. Besides bleeding complications, most directly linked to the procedure itself, the most common causes of death are related to non-protective mechanical ventilation or to infectious or non-infectious inflammation [5], leading to various degrees of organ dysfunction.
The aim of our study was to identify predictors of mortality in patients treated with ECMO in referral centers and to develop a score in order to better allocate resources and to define the best timing of ECMO institution.
Materials and methods
Ethical aspects
The present study is in compliance with the Declaration of Helsinki. In all patients ECMO was started emergently, and informed consent was waived according to Italian legislation. Individual data were anonymous according to the health ministry mandate for epidemiological and outcome surveillance of the ECMOnet program. The approval of the local ethics committees was therefore waived with no further informed consent required from the patients.
Study design
The data set from the ECMOnet was used to set up a prospective multicenter cohort study. The ECMOnet is a national network that includes all severely ill patients with suspected H1N1 virus infection admitted to the intensive care units (ICU) of 14 Italian tertiary care centers, endorsed and supported by the Italian Ministry of Health [6]. The ECMOnet data set collected the epidemiological and clinical features, treatment data and outcomes of 60 patients with ARDS suffering from confirmed or suspected H1N1 influenza A who received ECMO according to predefined ECMOnet eligibility criteria between August 2009 and March 2010 [6].
Data set
Baseline parameters were collected before ECMO cannulation. All patients with severe ARDS related to suspected H1N1 influenza A were included if at least one of the inclusion criteria was fulfilled despite the use of available rescue therapies: oxygenation index (OI) > 30, PaO2/FiO2 < 70 with PEEP ≥ 15 cmH2O (in patients already admitted to one of the ECMOnet centers) or PaO2/FiO2 < 100 with PEEP ≥ 10 cmH2O (in patients still to be transferred), pH < 7.25 for at least 2 h or hemodynamic instability. Exclusion criteria were intracranial bleeding or another major contraindication to anticoagulation, pre-existing severe disability and poor prognosis because of the underlying disease. Mechanical ventilation for more than 7 days was considered a relative exclusion criterion [6].
Patients and procedures
All 60 adult patients were admitted to the ICU of 1 of the 14 Italian tertiary care centers. The ECMO circuit setup consisted of a centrifugal pump and a coated polymethylpentene oxygenator. Percutaneous cannulation was performed using the Seldinger technique: 59 patients received VV ECMO (femoral-jugular in 27 cases, femoral–femoral in 26, jugular–jugular in 6); in 1 patient VV ECMO was initiated and sequentially transitioned to VA ECMO triggered by refractory hemodynamic impairment. All patients received intravenous continuous infusion of unfractionated heparin, antiviral therapy with Oseltamivir 150 mg twice a day and broad-spectrum antibiotics.
Statistical analysis
Continuous variables are reported as mean ± standard deviation or median and interquartile range, whereas categorical variables are reported as absolute numbers and percentages. Unadjusted univariate analyses were based on the Mann-Whitney U or median test and Fisher's exact test, respectively, with the computation of 95 % confidence intervals. For building a model predicting intrahospital mortality, multivariable analyses were performed. In detail, we modeled data using generalized estimating equations (GEE) to consider correlating features within the center, assuming the same correlation between any two elements of a cluster (exchangeable correlation matrix) [7, 8]. As the performance of the multivariate model depends on the initial number of variables [9], we included all the variables that were statistically associated with a p value ≤0.25 in the univariate models. In addition, we compared models within a nested subgroup of selected variables by quasi-likelihood under the independence model criterion (QIC) [10]. We started with factors revealing high significance (p = 0.01) in the univariate model and proceeded with forward selection. In multivariate regression, statistical significance was set at the two-tailed 0.05 level. When GEE regression coefficients could not be estimated (i.e., in case the generalized Hessian matrix was not positively definite) [11], we limited the analysis to the association performed by the Fisher exact test or Mann-Whitney U test for categorical or continuous variables, respectively.
Based on the coefficients of the multivariate analysis, we combined predictors for the assessment of mortality risk in patients who presented as ECMO candidates into a new score—the ECMOnet score. With the aim to be as intuitive as possible, the score was constructed to give a result between 0 and 10. Thus, the number resulting from score calculation can be easily associated with the mortality risk. In addition, each of the five parameters is given weight by the value measured (partial score). The partial score for each parameter was established according to its frequency distribution and its weight in the final GEE model. The ECMOnet score can be calculated with the following formula where ps i is the partial score assigned to each parameter.
The goodness-of-fit of the model, plotting mortality status versus ECMOnet score, was confirmed by the GEE model and QIC statistic. Besides, c-statistics (area under ROC curve) were calculated as a measure of a model’s ability to discriminate between survivors and non-survivors [12]. From the ROC curve analysis, the best cutoff value was identified as the point with the highest value sensitivity and specificity (Youden index: SE + SP − 1) [13]. The 95 % confidence interval for accuracy, sensitivity and specificity was calculated with normal approximation. In order to provide further external validation of the accuracy of the ECMOnet score, we used an external test set containing 74 patients suffering from ARDS because of H1N1 who received ECMO treatment in other countries [5, 14] or in the Italian ECMOnet centers during the 2010 H1N1 influenza A epidemics. The full data set was available for 60 patients in the validation group. Fifty-nine patients received VV ECMO, and one patient received VA ECMO. Four were converted from VV to VA ECMO because of circulatory failure during treatment [14].
Two examples of the ECMOnet score calculation on paradigmatic clinical cases are also available as supplementary online material.
Statistical significance was set at the two-tailed 0.05 level for all hypothesis testing. Data were analyzed with SAS 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
Among the 60 patients of the 2009 H1N1 pandemic, 49 (82 %) had confirmed H1N1-associated ARDS with a survival rate of 71 %. The remaining 11 (18 %) patients without confirmed H1N1-associated ARDS presented a survival rate of 54 %. Twenty-eight patients were referred from remote hospitals to the ECMOnet referral centers and treated with ECMO.
Multiple organ failure associated with sepsis was the most common cause of death (53 %), followed by septic shock (26 %). All nonsurvivors were still on ECMO at the time of death.
As shown in Table 1, all baseline characteristics, clinical parameters and vital signs were tested by univariate analysis. Using multivariate analysis, we identified five statistically significant predictors of death: bilirubin value (OR = 2.32, 95 % CI 1.52–3.52, p < 0.001), systemic mean arterial pressure (OR = 0.92, 95 % CI 0.88–0.97, p < 0.001), hematocrit value (OR = 0.82, 95 % CI 0.72–0.94, p = 0.006), preECMO hospital length of stay (OR = 1.52, 95 % CI 1.12–2.07, p = 0.008) and creatinine level (OR = 7.38, 95 % CI 1.43–38.11, p = 0.02).
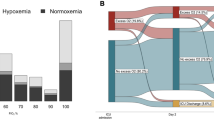
These five parameters were then entered into the ECMOnet score (Table 2). When evaluated in the univariate GEE model, the ECMOnet score was a statistically significant predictor of mortality (OR = 3.44, 95 % CI 2.04–5.81, p < 0.001). The ROC analysis further confirmed the high accuracy of the ECMOnet score (c = 0.857, 95 % CI 0.754–0.959, p < 0.001) for the prediction of the mortality risk in patients on ECMO. An ECMOnet score of 4.5 was found to be the most appropriate cutoff for mortality risk prediction. The probability of correctly classifying patients with the ECMOnet score is 75 % (95 % CI 64–87 %). In comparison, the SOFA (c = 0.711, 95 % CI 0.565–0.856, p = 0.005) and Murray scores (c = 0.581, 95 % CI 0.436–0.726, p = 0.3) revealed a lower performance in the evaluation of pre-implant mortality risk compared to the ECMOnet score.
We further analyzed the performance of the ECMOnet score to the subgroups of patients referred or not referred from remote hospitals. Not only was the prediction of mortality risk excellent in the 49 patients with H1N1 infection (c = 0.905, 95 % CI 0.820–0.991, p < 0.001), but also the ECMOnet score performed well in both groups of patients (n = 28), referred (c = 0.833, 95 % CI 0.630–0.999, p = 0.001) or not referred (n = 32) from remote hospitals (c = 0.838, 95 % CI 0.693–0.984, p < 0.001).Furthermore, we examined the reliability of the ECMOnet score by an external validation analysis: the validation group consisted of 74 patients with ARDS (45 male and 29 female), of whom 81 % (60/74) had confirmed H1N1 infection, and 57 % (42/74) were transferred from remote hospitals to the tertiary referral centers after the initiation of treatment with extracorporeal support. Mean age was 45 ± 14 years; overall survival rate was 49 % (36/74).The ROC analysis (Fig. 1) of this external test set revealed a strong capacity of the ECMOnet score to distinguish survivors from nonsurvivors (c = 0.694, 95 % CI 0.562–0.826, p = 0.004). The accuracy was 62 % (95 % IC 49–74 %), and sensitivity and specificity were 51 % (95 % IC 35–68 %) and 76 % (95 % IC 59–93 %), respectively.
Discussion
This study shows that mortality of adult patients suffering from influenza A (H1N1)-related ARDS undergoing VV ECMO is related to extrapulmonary organ function at the time of cannulation. PreECMO hospital length of stay; creatinine, bilirubin and hematocrit values; and systemic mean arterial pressure were significantly associated with mortality as assessed by multivariate analysis, while respiratory parameters were not associated with survival. To improve risk stratification and prediction of mortality risk at the time of VV ECMO initiation, we developed a multifactorial scoring system—the ECMOnet score.
Up to now, most data explaining the rates and causes of death refer to the time point after the start of ECMO: in a large multicenter database of 1,473 adult patients supported with ECMO for respiratory failure, survival at hospital discharge was 50 % [4]. Non-survivors displayed a higher rate of complications, including mechanical circuit complications; renal complications; surgical, GI and pulmonary hemorrhages; hyperglycemia, infections, arrhythmias and pneumothorax [4]. In a population of 137 pediatric patients undergoing VA ECMO, Morris and colleagues found that the development of renal and hepatic dysfunction during ECMO predicted mortality in postoperative patients with statistical significance [15]. Recently, Smalley et al. [16] performed a retrospective study on 50 children with pneumonia and managed with ECMO. In their study, the need to change the ECMO circuit and the need for continuous renal replacement therapy were predictors of death. Wagner et al. [17] found that, among 26 risk factors analyzed in a total of 72 patients receiving pulmonary ECMO, only preECMO serum creatinine levels correlated with survival. This result is in line with our findings, even if in their study adults, children and neonates suffering from different pulmonary diseases and treated with either VV or VA ECMO were all analyzed as a unique study group.
However, studies on this topic are few and potentially biased by the multiple etiologies of respiratory failure. In contrast, our patients presented as an homogeneous population with H1N1-associated pneumonia (confirmed in 81.7 %) referred to tertiary ECMO centers.
Furthermore, patients enrolled in our study were stringently treated with VV ECMO according to a national protocol with definite inclusion and exclusion criteria. Accordingly patient management was similar in the 14 tertiary centers, as the ECMOnet organized multiple ECMO training courses open to physicians, perfusionists and nurses [18]. The parameters identified in our study are very simple to implement clinically, and the use of the ECMOnet score for the evaluation of critically ill patients for VV ECMO institution can be applied easily to patients referred from remote hospitals. External validation indicates that the information provided by the ECMOnet score is statistically robust in further patient groups.
The potential benefits of the new score, however, may be not limited to the setting of H1N1 influenza A virus-related acute lung failure. After further validation in different settings of acute respiratory distress syndrome, endorsing this score in clinical practice would allow cannulation of patients in the presence of organ dysfunction before strict respiratory criteria are met and refusal of ECMO in patients with high predicted mortality.
Protective ventilation was shown to improve survival in patients with ARDS by the ARDS network [19]. Besides its lung-protective effects, the favorable effects of ECMO appear to be related to its beneficial hemodynamic impact on preserving distal perfusion (i.e., kidney, liver), particularly if focusing on causes of death.
ECMO is safer, cheaper and simpler than in previous eras [20]. While the CESAR trial showed an improvement in survival [1], the ECMOnet experience demonstrated that its application is feasible and effective [6]. Moreover, the ECMOnet data set analysis allowed the development of the ECMOnet score, and the validation analysis revealed a potentially strong impact on clinical practice.
Some limitations of this study should be acknowledged. First, complications occurring during ECMO have a strong impact on the outcome, and these are not addressed with baseline parameters. Our study used predefined indications for ECMO based on gas exchange and ventilator pressure, which are not universally standardized and remain an important matter of discussion. Another limitation is the inability to provide a distinction between patients with viral sepsis at baseline and those who had superinfection, as the majority of deaths in our population were related to multiple organ failure associated with sepsis and septic shock. However, the facts should not be underestimated that the overlap between shock, SIRS, ECMO itself and sepsis is always part of the clinical scenario in patients undergoing extracorporeal support [21] and that all patients were already septic at baseline. Finally, the accuracy of the ECMOnet score [62 % (95 % IC 49–74 %)], and the sensitivity and specificity [51 % (95 % IC 35–68 %) and 76 % (95 % IC 59–93 %), respectively] should be further validated in larger ARDS populations.
Conclusions
Our data provide new perspectives concerning the allocation of resources for VV ECMO. We confirm the strong clinical perception that survival is strongly correlated to extrapulmonary organ function at the time of ECMO initiation. This knowledge may help to identify potential candidates for ECMO support according to their mortality risk and provides guidance to solve crucial economic and ethical issues.
References
Peek GJ, Clemens F, Elbourne D, Firmin R, Hardy P, Hibbert C, Killer H, Mugford M, Thalanany M, Tiruvoipati R, Truesdale A, Wilson A (2006) CESAR: conventional ventilatory support vs extracorporeal membrane oxygenation for severe adult respiratory failure. BMC Health Serv Res 6:163. doi:10.1186/1472-6963-6-163
Davies A, Jones D, Balley M, Beca J, Bellomo R, Blackwell N, Forrest P, Gattas D, Granger E, Herkes R, Jackson A, McGuinness S, Nair P, Pellegrino V, Pettilä V, Plunkett B, Pye R, Torzillo P, Webb S, Wilson M, Ziegenfuss M, The Australia New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators (2009) Extracorporeal Membrane Oxygenation for 2009 Influenza A (H1N1) Acute respiratory distress syndrome. JAMA 302:1888–1895. doi:10.1001/jama.2009.1535
Noah MA, Peek GJ, Finney SJ, Griffiths MJ, Harrison DA, Grieve R, Sadique MZ, Sekhon JS, McAuley DF, Firmin RK, Harvey C, Cordingley JJ, Price S, Vuylsteke A, Jenkins DP, Noble DW, Bloomfield R, Walsh TS, Perkins GD, Menon D, Taylor BL, Rowan KM (2011) Referral to an extractorporeal membrane oxygenation center and mortality among patients with severe 2009 influenza A (H1N1). JAMA 306:1659–1668. doi:10.1001/jama.2011.1471
Brogan TV, Thiagarajan RR, Rycus PT, Bartlett RH, Bratton SL (2009) Extracorporeal membrane oxygenation in adults with severe respiratory failure: a multi-center database. Intensive Care Med 35:2105–2114. doi:10.1007/s00134-009-1661-7
Beutel G, Wiesner O, Eder M, Hafer C, Schneider AS, Kielstein JT, Kühn C, Heim A, Ganzenmüller T, Kreipe HH, Haverich A, Tecklenburg A, Ganser A, Welte T, Hoeper MM (2011) Virus-associated hemophagocytic syndrome as a major contributor to death in patients with 2009 influenza A (H1N1) infection. Crit Care 15:R80. doi:10.1186/cc10073
Patroniti N, Zangrillo A, Pappalardo F, Peris A, Cianchi G, Braschi A, Iotti GA, Arcadipane A, Panarello G, Ranieri VM, Terragni P, Antonelli M, Gattinoni L, Oleari F, Pesenti A (2011) The italian ECMO network experience during the 2009 influenza A(H1N1) pandemic: preparation for severe respiratory emergency outbreaks. Intensive Care Med 37:1447–1457
Liang KY, Zeger SL (1993) Regression analysis for correlated data. Annu Rev Public Health 14:43–68. doi:10.1146/annurev.pu.14.050193.000355
Liang K, Zeger SL (1986) Longitudinal data analysis using generalized linear models. Biometrika 73:13–22
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Pan W (2001) Akaike’s information criterion in generalized estimating equations. Biometrics 57:120–125
Gill J (2004) What to do when your hessian is not invertible: alternatives to model respecification in nonlinear estimation. Soc Methods Res 33:54–87
Obuchowski NA (2005) ROC analysis. AJR Am J Roentgenol 184:364–372
Fluss R, Faraggi D, Reiser B (2005) Estimation of the youden index and its associated cutoff point. Biom J 47:458–472
Holzgraefe B, Broomé M, Kalzén H, Konrad D, Palmér K, Frenckner B (2010) Extracorporeal membrane oxygenation for pandemic H1N1 2009 respiratory failure. Minerva Anestesiol 76:1043–1051
Morris MC, Ittenbach RF, Godinez RI, Portnoy JD, Tabbutt S, Hanna BD, Hoffman TM, Gaynor JW, Connelly JT, Helfaer MA, Spray TL, Wernovsky G (2004) Risk factors for mortality in 137 pediatric cardiac intensive care unit patients managed with extracorporeal membrane oxygenation. Crit Care Med 32:1061–1069. doi:10.1097/01.CCM.0000119425.04364.CF
Smalley N, MacLaren G, Best D, Paul E (2012) Butt W (2012) Outcomes in children with refractory pneumonia supported with extracorporeal membrane oxygenation. Intensive Care Med 38:1001–1007. doi:10.1007/s00134-012-2581-5
Wagner K, Risnes I, Abdelnoor M, Karlsen HM, Svennevig JL (2008) Is it possible to predict outcome in pulmonary ECMO? analysis of pre-operative risk factors. Perfusion 23:95–99. doi:10.1177/0267659108096260
Brazzi L, Lissoni A, Panigada M, Bottino N, Patroniti N, Pappalardo F, Gattinoni L (2012) Simulation-based training of extracorporeal membrane oxygenation (ECMO) during H1N1 influenza pandemic: the Italian experience. Simul Healthc 7:32–34. doi:10.1097/SIH.0b013e31823ebccb
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome: the acute respiratory distress syndrome network. N Engl J Med 342:1301–1308
MacLaren G, Combes A, Bartlett RH (2012) Contemporary extracorporeal membrane oxygenation for adult respiratory failure: life support in the new era. Intensive Care Med 38:210–220. doi:10.1007/s00134-011-2439-2
Pieri M, Greco T, De Bonis M, Maj G, Fumagalli L, Zangrillo A, Pappalardo F (2012) Diagnosis of infection in patients undergoing extracorporeal membrane oxygenation: a case-control study. J Thorac Cardiovasc Surg 143:1411–1416. doi:10.1016/j.jtcvs.2012.01.005
Acknowledgments
Members of the ECMOnet Italian ECMO network not included in the authors’ list: A.M. Scandroglio, M.G. Calabrò, T. Bove, M. De Bonis (Department of Cardiothoracic and Vascular Anesthesia and Intensive Care, San Raffaele Scientific Institute, Vita-Salute University, Milan, Italy); G. Foti, M. Bombino (Department of Perioperative Medicine and Intensive Care, San Gerardo Hospital, Monza, Italy); A. Peris, G. Cianchi, A. Pasquini (Department of Anesthesiology and Intensive Care, Carreggi University Hospital, Firenze, Italy); A. Braschi, F. Mojoli (Department of Anesthesiology and Intensive Care I, IRCCS Policlinico San Matteo Foundation, University of Pavia, Italy); M. Zanierato (Department of Anesthesiology and Intensive Care I, IRCCS Policlinico San Matteo Foundation, Italy); G.A. Iotti, M. Belliato, L. Carnevale (Department of Anesthesiology and Intensive Care II, IRCCS Policlinico San Matteo Foundation, University of Pavia, Italy); P. Terragni, R. Urbino, L. Del Sorbo, V. Fanelli (Department of Anesthesia and Critical Care Medicine, University of Turin, S. Giovanni Battista-Molinette Hospital, Turin, Italy); G. Panarello (Department of Intensive Care, Mediterranean Institute for Transplantation and Advanced Specialized Therapies, Palermo, Italy); M. Antonelli, G. Bello, R. Maviglia (Department of Anesthesiology and Intensive Care Medicine, Cattolica—Sacro Cuore University, Rome, Italy); A. Lissoni, S. Crotti (Department of Anesthesia, IRCCS Ca’ Granda Foundation Maggiore Policlinico Hospital, University of Milan, Milan, Italy); P. Pietropaoli, M. Rocco, A. Morelli (Department of Anesthesiology, Critical Care Medicine, and Pain Therapy, La Sapienza University, Rome, Italy); G. Frascaroli, F. Caramelli (Department of Cardio-thoraco-vascular Integrated Activities, S. Orsola-Malpighi University Hospital, Bologna, Italy); R. Tufano, M. Iannuzzi (Department of Anesthesiology, Resuscitation Care, Intensive Care, Hyperbaric Therapy, Pain Therapy, Federico II University, Naples, Italy); F. Bruno, S. Grasso (Anesthesiology and Intensive Care Unity, Department of Emergency Medicine and Organ Transplants, Bari University, Bari, Italy); L. Lorini (Department of Anesthesiology and Intensive Care, Ospedali Riuniti, Bergamo, Italy); C. Ori, S. Rossi, P. Persona (Institute of Anesthesiology and Intensive Care, University Hospital of Padua, Padua, Italy). The ECMOnet is a national network instituted by the Italian Ministry of Health in response to the 2009 H1N1 pandemic. The Italian Ministry of Health allocated all economic, human and technological resources required for the development and activity of the ECMOnet. Our study used the ECMOnet registry as the main data source. We did not receive funds from the Italian Ministry of Health for the present study. The analysis presented in this study was entirely supported by departmental funds. The authors had full control of primary data, and they agree to allow the journal to review their data if requested.
Author information
Authors and Affiliations
Consortia
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pappalardo, F., Pieri, M., Greco, T. et al. Predicting mortality risk in patients undergoing venovenous ECMO for ARDS due to influenza A (H1N1) pneumonia: the ECMOnet score. Intensive Care Med 39, 275–281 (2013). https://doi.org/10.1007/s00134-012-2747-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2747-1