Abstract
Objective
To determine, in the early stages of suspected clinically significant infection, the independent relationship of the presenting venous lactate level to 28-day in-hospital mortality.
Design
Prospective, observational cohort study.
Setting
Urban, university tertiary-care hospital.
Patients
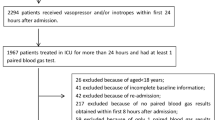
One thousand two hundred and eighty seven adults admitted through the emergency department who had clinically suspected infection and a lactate measurement.
Measurements and results
Seventy-three [5.7% (95% CI 4.4–6.9%)] patients died in the hospital within 28 days. Lactate level was strongly associated with 28-day in-hospital mortality in univariate analysis (p < 0.0001). When stratified by blood pressure, lactate remained associated with mortality (p < 0.0001). Normotensive patients with a lactate level ≥ 4.0 mmol/l had a mortality rate of 15.0% (6.0–24%). Patients with either septic shock or lactate ≥ 4.0 mmol/l had a mortality rate of 28.3% (21.3–35.3%), which was significantly higher than those who had neither [mortality of 2.5% (1.6–3.4%), p < 0.0001]. In a model controlling for age, blood pressure, malignancy, platelet count, and blood urea nitrogen level, lactate remained strongly associated with mortality. Patients with a lactate level of 2.5–4.0 mmol/l had adjusted odds of death of 2.2 (1.1–4.2); those with lactate ≥ 4.0 mmol/l had 7.1 (3.6–13.9) times the odds of death. The model had good discrimination (AUC = 0.87) and was well calibrated.
Conclusions
In patients admitted with clinically suspected infection, the venous lactate level predicts 28-day in-hospital mortality independent of blood pressure and adds significant prognostic information to that provided by other clinical predictors.

Similar content being viewed by others
References
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29:1303–1310
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Brun-Buisson C, Meshaka P, Pinton P, Vallet B (2004) EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med 30:580–588
Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, Artigas A, Sicignano A, Palazzo M, Moreno R, Boulme R, Lepage E, Le Gall R (2002) Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med 28:108–121
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall JC, Parker MM, Ramsay G, Zimmerman JL, Vincent JL, Levy MM (2004) Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 32:858–873
Shapiro NI, Howell MD, Talmor D, Lahey D, Ngo L, Buras J, Wolfe RE, Weiss JW, Lisbon A (2006) Implementation and outcomes of the Multiple Urgent Sepsis Therapies (MUST) protocol. Crit Care Med 34:1025–1032
Kortgen A, Niederprum P, Bauer M (2006) Implementation of an evidence-based “standard operating procedure” and outcome in septic shock. Crit Care Med 34:943–949
Ander DS, Jaggi M, Rivers E, Rady MY, Levine TB, Levine AB, Masura J, Gryzbowski M (1998) Undetected cardiogenic shock in patients with congestive heart failure presenting to the emergency department. Am J Cardiol 82:888–891
Rady MY, Rivers EP, Nowak RM (1996) Resuscitation of the critically ill in the ED: responses of blood pressure, heart rate, shock index, central venous oxygen saturation, and lactate. Am J Emerg Med 14:218–225
Meregalli A, Oliveira RP, Friedman G (2004) Occult hypoperfusion is associated with increased mortality in hemodynamically stable, high-risk, surgical patients. Crit Care 8:R60–65
Shapiro NI, Howell MD, Talmor D, Nathanson LA, Lisbon A, Wolfe RE, Weiss JW (2005) Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med 45:524–528
Lavery RF, Livingston DH, Tortella BJ, Sambol JT, Slomovitz BM, Siegel JH (2000) The utility of venous lactate to triage injured patients in the trauma center. J Am Coll Surg 190:656–664
Myint PK, Kamath AV, Vowler SL, Maisey DN, Harrison BD (2005) The CURB (confusion, urea, respiratory rate and blood pressure) criteria in community-acquired pneumonia (CAP) in hospitalised elderly patients aged 65 years and over: a prospective observational cohort study. Age Ageing 34:75–77
Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW (2003) Mortality in Emergency Department Sepsis (MEDS) score: a prospectively derived and validated clinical prediction rule. Crit Care Med 31:670–675
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Blow O, Magliore L, Claridge JA, Butler K, Young JS (1999) The golden hour and the silver day: detection and correction of occult hypoperfusion within 24 hours improves outcome from major trauma. J Trauma 47:964–969
Crowl AC, Young JS, Kahler DM, Claridge JA, Chrzanowski DS, Pomphrey M (2000) Occult hypoperfusion is associated with increased morbidity in patients undergoing early femur fracture fixation. J Trauma 48:260–267
Broder G, Weil MH (1964) Excess lactate: an index of reversibility of shock in human patients. Science 143:1457–1459
Bossink AW, Groeneveld AB, Koffeman GI, Becker A (2001) Prediction of shock in febrile medical patients with a clinical infection. Crit Care Med 29:25–31
Claridge JA, Crabtree TD, Pelletier SJ, Butler K, Sawyer RG, Young JS (2000) Persistent occult hypoperfusion is associated with a significant increase in infection rate and mortality in major trauma patients. J Trauma 48:8–14; discussion 15
Wo CC, Shoemaker WC, Appel PL, Bishop MH, Kram HB, Hardin E (1993) Unreliability of blood pressure and heart rate to evaluate cardiac output in emergency resuscitation and critical illness. Crit Care Med 21:218–223
Bakker J (2001) Lactate: may I have your votes please? Intensive Care Med 27:6–11
Levraut J, Ichai C, Petit I, Ciebiera JP, Perus O, Grimaud D (2003) Low exogenous lactate clearance as an early predictor of mortality in normolactatemic critically ill septic patients. Crit Care Med 31:705–710
Astiz M, Rackow EC, Weil MH, Schumer W (1988) Early impairment of oxidative metabolism and energy production in severe sepsis. Circ Shock 26:311–320
Levraut J, Ciebiera JP, Chave S, Rabary O, Jambou P, Carles M, Grimaud D (1998) Mild hyperlactatemia in stable septic patients is due to impaired lactate clearance rather than overproduction. Am J Respir Crit Care Med 157:1021–1026
Mizock BA, Falk JL (1992) Lactic acidosis in critical illness. Crit Care Med 20:80–93
Bakker J, Coffernils M, Leon M, Gris P, Vincent JL (1991) Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock. Chest 99:956–962
Bakker J, Gris P, Coffernils M, Kahn RJ, Vincent JL (1996) Serial blood lactate levels can predict the development of multiple organ failure following septic shock. Am J Surg 171:221–226
Varpula M, Tallgren M, Saukkonen K, Voipio-Pulkki LM, Pettila V (2005) Hemodynamic variables related to outcome in septic shock. Intensive Care Med 31:1066–1071
Husain FA, Martin MJ, Mullenix PS, Steele SR, Elliott DC (2003) Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg 185:485–491
McNelis J, Marini CP, Jurkiewicz A, Szomstein S, Simms HH, Ritter G, Nathan IM (2001) Prolonged lactate clearance is associated with increased mortality in the surgical intensive care unit. Am J Surg 182:481–485
Jeng JC, Jablonski K, Bridgeman A, Jordan MH (2002) Serum lactate, not base deficit, rapidly predicts survival after major burns. Burns 28:161–166
Cerovic O, Golubovic V, Spec-Marn A, Kremzar B, Vidmar G (2003) Relationship between injury severity and lactate levels in severely injured patients. Intensive Care Med 29:1300–1305
Asimos AW, Gibbs MA, Marx JA, Jacobs DG, Erwin RJ, Norton HJ, Thomason M (2000) Value of point-of-care blood testing in emergent trauma management. J Trauma 48:1101–1108
Jones AE, Fitch MT, Kline JA (2005) Operational performance of validated physiologic scoring systems for predicting in-hospital mortality among critically ill emergency department patients. Crit Care Med 33:974–978
Nguyen HB, Rivers EP, Havstad S, Knoblich B, Ressler JA, Muzzin AM, Tomlanovich MC (2000) Critical care in the emergency department: a physiologic assessment and outcome evaluation. Acad Emerg Med 7:1354–1361
Vincent JL, Yagushi A, Pradier O (2002) Platelet function in sepsis. Crit Care Med 30:S313–317
Yegenaga I, Hoste E, Van Biesen W, Vanholder R, Benoit D, Kantarci G, Dhondt A, Colardyn F, Lameire N (2004) Clinical characteristics of patients developing ARF due to sepsis/systemic inflammatory response syndrome: results of a prospective study. Am J Kidney Dis 43:817–824
Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, Lewis SA, Macfarlane JT (2003) Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 58:377–382
Society BT. BTS Guidelines for the management of community acquired pneumonia in adults – 2004 update. 2004 April 4, 2004 [cited 2006 October 1, 2006]; available from: http://www.brit-thoracic.org.uk/c2/uploads/MACAPrevisedApr04.pdf
Shapiro NI, Howell M, Talmor D (2005) A blueprint for a sepsis protocol. Acad Emerg Med 12:352–359
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-007-0679-y
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Howell, M.D., Donnino, M., Clardy, P. et al. Occult hypoperfusion and mortality in patients with suspected infection. Intensive Care Med 33, 1892–1899 (2007). https://doi.org/10.1007/s00134-007-0680-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0680-5