Abstract
Objective
Colonization of multiple body sites is a leading risk factor for Candida spp. infection in intensive care unit (ICU) patients. We evaluated whether oral nystatin prophylaxis reduces Candida spp. colonization in ventilated ICU patients.
Design and setting
Prospective, randomized, open-label study with blinded assessment of the objective primary evaluation criterion in the medical-surgical ICU of a teaching hospital.
Patients
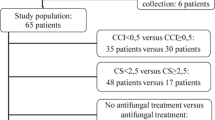
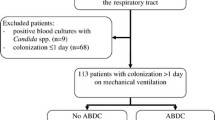
The study included 98 consecutive patients mechanically ventilated for at least 48 h (mean age 58±19 years; mean SAPS II 40±11), assigned to either treatment group (n=51) or control group (n=47). Study groups were comparable for age, SAPS II, reason for admission, and immune status.
Interventions
Patients were randomized to receive oral nystatin (treatment group; 3×106 U per day) or no nystatin (control group). Multiple body sites (trachea, stomach, rectum, urine, groin, and blood) were tested for Candida spp. on admission and then every 3 days by mycologists blinded to group assignment, and the colonization index was determined.
Results
Colonization by Candida spp. developed in 25% of controls but in none of the treated patients. In multivariate analysis, the absence of nystatin prophylaxis and ICU length of stay were independently associated with Candida spp. colonization. No invasive candidiasis was diagnosed in either study group.
Conclusions
Oral nystatin prophylaxis efficiently prevented Candida spp. colonization in ICU patients at low risk of developing invasive candidiasis. Further studies are needed to determine whether this strategy remains efficient in reducing Candida spp. infections in higher risk ICU patients.



Similar content being viewed by others
References
Martin GS, Mannini DM, Eaton S, Moss M (2003) The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 348:1546–1554
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24, 179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39:309–317
Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH, Wolff M, Spencer RC, Hemmer M (1995) The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) study. JAMA 274:639–644
Eggimann P, Garbino J, Pittet D (2003) Epidemiology of Candida species infections in critically ill non-immunosuppressed patients. Lancet Infect Dis 3:685–702
Nucci M, Anaissie E (2001) Revisiting the source of candidemia: skin or gut? Clin Infect Dis 33:1959–1967
Voss A, Hollis RJ, Pfaller MA, Wenzel RP, Doebbeling BN (1994) Investigation of the sequence of colonization and candidemia in nonneutropenic patients. J Clin Microbiol 32:975–980
Pittet D, Monod M, Suter PM, Frenk E, Auckenthaler R (1994) Candida colonization and subsequent infections in critically ill surgical patients. Ann Surg 220:751–758
Solomkin JS, Flohr AB, Quie PG, Simmons RL (1980) The role of Candida in intraperitoneal infections. Surgery 88:524–530
Rex JH, Walsh TJ, Sobel JD, Filler SG, Pappas PG, Dismukes WE, Edwards JE (2000) Practice guidelines for the treatment of Candidiasis. Clin Infect Dis 30:662–678
Eggimann P, Garbino J, Pittet D (2003) Management of Candida species infections in critically ill patients. Lancet Infect Dis 3:772–785
Rex JH, Sobel JD (2001) Prophylactic antifungal therapy in the intensive care unit. Clin Infect Dis 32:1191–1200
Azoulay E, Schlemmer B (2004) Faut-il proposer une prophylaxie antifungique aux patients non neutropéniques de réanimation? Réanimation 13:87–92
Jacobs S, Price Evans DA, Tariq M, Al Omar NF (2003) Fluconazole improves survival in septic shock: a randomized double-blind prospective study. Crit Care Med 31:1938–1946
Garbino J, Lew DP, Romand JA, Hugonnet S, Auckenthaler R, Pittet D (2002) Prevention of severe Candida infections in nonneutropenic, high-risk, critically ill patients: a randomized, double-blind, placebo-controlled trial in patients treated by selective digestive decontamination. Intensive Care Med 28:1708–1717
Desai MH, Rutan RL, Heggers JP, Herndon DN (1992) Candida infection with and without nystatin prophylaxis: a 11-year experience with patients with burn injury. Arch Surg 127:159–162
Cerra FB, Maddaus MA, Dunn DL, Wells CL, Konstantinides NN, Lehmann SL, Mann HJ (1992) Selective gut decontamination reduces nosocomial infections and length of stay but not mortality or organ failure in surgical intensive care unit patients. Arch Surg 127:163–167
Savino JA, Agarwal N, Wry P, Policastro A, Cerabona T, Austria L (1994) Routine prophylactic antifungal agents (clotrimazole, ketoconazole, and nystatin) in nontransplant/nonburned critically ill surgical and trauma patients. J Trauma 36:20–25
Petri MG, König J, Moecke HP, Gramm HJ, Barkow H, Kujath P, Dennhart R, Schäfer H, Meyer N, Kalmar P, Thülig P, Müller J, Lode H, Paul-Ehrlich Society for Chemotherapy, Divisions of Mycology and Pneumonia Research (1997) Intensive Care Med 23:317–325
McKinnon PS, Goff DA, Kern JW, Devlin JW, Barletta JF, Sierawski SJ, Mosenthal AC, Gore P, Ambegaonkar AJ, Lubowski TJ (2001) Temporal assessment of Candida risk factors in the surgical intensive care unit. Arch Surg 136:1401–1408
Charles PE, Dalle F, Aube H, Doise JM, Quenot JP, Aho LS, Chavanet P, Blettery B (2005) Candida spp. colonization significance in critically ill medical patients: a prospective study. Intensive Care Med 31:393–400
Régnier B, Attal M, Bezie Y, Blanc V, Buzyn A, Choutet P, Mimoz O, Papazian L, Pialoux G, Pottecher T, Poyart C, Tazi A, Tilleul P (2004) Prise en charge des aspergilloses et candidoses invasives de l’adulte. Réanimation 13:5–13
Gotzsche PC, Johansen HK (2002) Nystatin prophylaxis and treatment in severely immunodepressed patients. Cochrane Database Syst Rev 4:CD002033
Acknowledgements
We gratefully thank Pr. Didier Pittet for his expertise and constructive critique of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-005-2806-y
Rights and permissions
About this article
Cite this article
Normand, S., François, B., Dardé, ML. et al. Oral nystatin prophylaxis of Candida spp. colonization in ventilated critically ill patients. Intensive Care Med 31, 1508–1513 (2005). https://doi.org/10.1007/s00134-005-2807-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2807-x