Abstract
Objective
To determine the threshold of age that best discriminates the survival of mechanically ventilated patients and to estimate the outcome of mechanically ventilated older patients.
Design
International prospective cohort study.
Setting
Three hundred sixty-one intensive care units from 20 countries.
Patients and participants
Five thousand one hundred eighty-three patients mechanically ventilated for more than 12 h.
Interventions
None.
Measurements and results
Recursive partitioning and logistic regression were used and an outcome model was derived and validated using independent subgroups of the cohort. Two age thresholds (43 and 70 years) were found, by partitioning recursive analysis, to be associated with outcome. This study focuses on the analysis of patients older than 43 years of age, divided in two subgroups: between 43 and 70 years (middle age group) and older than 70 years (elderly group). Survival in hospital was 45% (95% C.I.: 43–48) for the elderly group and 55% (53–57) for the middle age group (p<0.001). Advanced age was not associated with prolongation of mechanical ventilation, weaning or length of stay in the ICU and in hospital (p>0.05). Variables associated with mortality in the elderly were: acute renal failure, shock, Simplified Acute Physiology Score II and a ratio of PaO2 to FIO2 more than 150.
Conclusions
Older mechanically ventilated patients (age >70 years) had a lower ICU and hospital survival, but the duration of mechanical ventilation, ICU and hospital stay were similar to younger patients. Factors associated with the highest risk of mortality in patients older than 70 were the development of complications during the course of mechanical ventilation, such as acute renal failure and shock.
Similar content being viewed by others
Introduction
Life expectancy continues to increase and, as a consequence, there are more patients who require access to the intensive care unit (ICU) [1]. Patients over 65 years account for a large proportion of healthcare expenditure [2, 3, 4, 5, 6, 7]. Indeed, nearly two-thirds of all ICU days are devoted to caring for patients older than 65 years of age [8].
A number of investigators have recently examined the effect of age on the outcomes of mechanically ventilated patients [4, 9, 10, 11, 12, 13, 14, 15]. Many of these investigations were limited, however, by a retrospective design, a small sample size, the lack of a generalized population of ventilated patients or the failure to adjust for baseline severity of disease. Moreover, the definition of the term “elderly” has varied between 60 and 80 years of age [9, 15, 16, 17, 18].
A number of questions relating to age and mechanical ventilation remain incompletely answered. Three such questions are the focus of this paper: (1) Is there a threshold of age associated with a lower survival in ventilated patients that might be helpful for analyzing the outcomes of future clinical trials? (2) Do older patients consume more resources or receive greater intensity of care? and (3) Are there specific variables associated with adverse outcomes in older patients with respiratory failure? To address these questions, analyses were conducted of the data collected in a prospective observational study (the largest heterogeneous population of mechanically ventilated patients reported to date [19]).
Material and methods
The database of the International Mechanical Ventilation Study [19], which was collected in March, 1998, was analyzed. The following information was collected on each patient receiving mechanical ventilation: demographic data, type of problem (medical or surgical), date of initiation of mechanical ventilation, primary indication for mechanical ventilation and issues related to patient management. Development of the following events was assessed daily during the course of mechanical ventilation for a maximum of 28 days: acute respiratory distress syndrome (ARDS), barotrauma, pneumonia, sepsis, renal failure, hepatic failure and coagulopathy. Sepsis, pneumonia and ARDS were considered as events only if they appeared more than 48 h after the initiation of mechanical ventilation. A patient was considered to have any of the above conditions if it was present for at least two consecutive days. Each of these conditions has been previously defined [19]. The arterial blood gases correspond to the values obtained once daily at approximately 8:00 a.m. The ventilator variables correspond to the time that the arterial blood gases were obtained. The use of neuromuscular blockers, sedatives and vasoactive drugs (given for at least 3 h in a 24-h period) was recorded daily for a maximum of 28 days. Weaning refers to the discontinuation of mechanical ventilation. The onset for this was the time when the physician in charge considered the patient was likely to be able to resume spontaneous breathing.
In terms of statistical analysis, the results are expressed as means and standard deviations, median with the interquartile range and proportions as appropriate. Student’s t-test or Mann-Whitney U test were used to compare continuous variables and chi-square test or Fisher’s test were used to compare proportions. The association of mortality and age was quantified and tested using the Spearman rank correlation coefficient.
A recursive partitioning method [20] was first used to look for the threshold of age that best discriminated for ICU survival. Two statistical methods, recursive partitioning and logistic regression, were then used to analyze the data corresponding to the group older than 70 years in Europe (derivation group, n=849). The derivation models that provided the best fit for elderly patients in Europe were then applied as a validation set to patients from USA-Canada (n=498) and Latin-America (n=265). First, a classification tree was constructed using the recursive partitioning procedure (Answer Tree Software, Chicago, Illinois) and the following variables: age, Simplified Acute Physiological Score (SAPS) II, sex, previous functional status, principal reason for initiating the mechanical ventilation, variables associated with patient management (such as successful non-invasive ventilation, use of non-conventional techniques—prone position, inhaled nitric oxide, permissive hypercapnia, inverse ratio ventilation—need of neuromuscular blockers, need of sedatives, tidal volume, respiratory rate, applied positive end-expiratory pressure, peak pressure, plateau pressure, tracheostomy), complications while receiving mechanical ventilation (such as barotrauma, ARDS, sepsis, pneumonia, shock, acute renal failure, hepatic failure, coagulopathy, metabolic acidosis, respiratory acidosis, ratio of partial pressure of oxygen to fraction of inspired oxygen, PaO2:FIO2).
The recursive partitioning method identified the threshold value for each variable that provided the best separation of the study population according to survival. For continuous variables, potential threshold values are all the values represented in the data. For dichotomous variables, the threshold value is the integer value of the two categories. For non-ordered categorical variables that have more than two categories, all factorial arrangements of the category were evaluated. For each variable, the program selected the threshold value that produced two subsets of the greatest purity. The partitioning was started after evaluating each risk variable for its ability to separate cases from controls. The variable that achieved the most precise separation of dead from living patients was selected as the best predictor for the first branch of the tree. The recursive partitioning procedure was repeated for each of the two subgroups that resulted from the first split, again searching all the cut-off points of each separation of dead and alive groups. The process was repeated for subsequent descendant subsets until no further partitioning was feasible because the subgroup contained fewer than 25 patients or contained only dead or only alive patients. The purpose of this classification tree was to reveal the structure of the database with respect to distinct combinations of variables that jointly influence the risk of mortality.
Second, the distinct risk subgroups identified by the classification tree were modeled using logistic regression. A dummy variable with different risk subgroups represented by the subsets at the bottom of the classification tree was introduced in a logistic regression analysis to estimate the odds ratios for the mortality of each subgroup in relation to the subgroup with a lower mortality. This model was validated in the Latin-America and USA-Canada cohorts (validation group) and the goodness-of-fit of this model was checked with Hosmer-Lemeshow’s test.
Results
Is there a threshold age associated with a lower survival in ventilated patients?
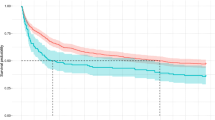
Our analysis identify that patients younger than 43 years showed the highest survival, then those in the group aged 43–70 years and the lowest survival was in patients more than 70 years the age (Fig. 1). The distribution of the 5,183 patients in the three age groups was as follows: 1,612 patients older than 70 years (31%), 2,506 patients between 43 and 70 years (48%) and 1,057 patients less than 43 years old (20%). For the purpose of this study, additional analysis was focused on the group older than 43 years, divided into two subgroups: between 43 and 70 years (middle age group) and older than 70 years (elderly group).
Recursive partitioning analysis to know the best age thresholds that discriminated survival. The first split of the patients showed that 43 years was the best threshold value. Subsequent split showed that in the group higher than 43 years, a age of 70 years separated two groups with different survival rates. Comparison of survival between three final nodes (≤ 43 years, between 43 and 70 years and >70 years) was statistically significant (Spearman’s test, p<0.001)
Both ICU survival and hospital survival decreased with increasing age (Spearman r=0.19, p<0.001). The survival in the ICU of patients older than 70 years was 63% (CI 95%: 61–65) and survival of patients between 43 and 70 years was 69% (68–71, p<0.001). Survival in hospital was 45% (43–48) for patients more than 70 years and 55% (53–57) for patients between 43 and 70 years (p<0.001).
Do older patient consume greater intensity of care?
Table 1 shows demographic characteristics and the principal reason for mechanical ventilation. The group older than 70 years included more women and more patients with limited activity before admission to hospital. Despite the difference in age dictated by the groupings, the severity of illness estimated by the modified SAPS II score was lower in the older population. Differences were found among patients between 43 and 70 years and patients older than 70 years (p<0.001) in the principal reason for mechanical ventilation: older patients were ventilated because of cardiac diseases (heart failure and cardiac arrest) and fewer were ventilated because of coma, ARDS and trauma (p<0.001).
In the management of the patients during mechanical ventilation (Table 2) significant differences were found in the use of positive end-expiratory pressure above 10 cmH20 (p<0.001) and neuromuscular blockers (p<0.001) in the older patients.
There were no significant differences in the rate of scheduled extubation between age groups (p=0.30). In the elderly group, 857 patients (53%, CI 95% 51–56) were extubated versus 1,374 patients (55%; 53–57) in the group between 43 and 70 years. Rate of reintubation was: 17% (14–19) in the elderly group and 14% (12–16) in the middle age group (p=0.04). There were no significant differences in the rate of accidental extubation: 43 patients (3%, 2–4) in patients over 70 years and 86 patients (3%, 3–4) in the age group from 43 to 70 years (p=0.16) or in the rate of reintubation of these patients who were accidentally extubated: 49% (33–64) and 38% (28–49), respectively (p=0.25).
The rate of tracheostomy was similar in the two groups (p=0.15) with a rate of 10% (8–11) in the elderly group and 12% (10–13) in the middle age group The tracheostomy was performed at a median time of 13 days (25th and 75th percentiles were 8.5 and 18) in the patients older than 70 years and of 11 days (7 and 16) in the middle age group (p=0.04).
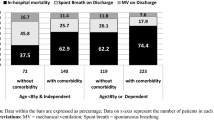
Table 3 shows the incidence of events that occurred over the course of mechanical ventilation. Older patients had a higher incidence of shock and acute renal failure (p<0.001). The older patients (survivors and non-survivors) had a similar duration of mechanical ventilation, weaning, length of stay in the ICU and length of stay in the hospital (Fig. 2).
Comparison of the time of ventilatory support (days of mechanical ventilation and days of weaning) and time of stay in the intensive care unit and in the hospital between patients aged from 43 to 70 years (middle age group) and patients older than 70 years (elderly group). The white boxes correspond to patients who survive and the grey boxes to non-survivors. Box plot indicates the median and the interquantile range. Bar indicates the minimum and the maximum number of days
Are there specific variables associated with adverse outcomes in those over 70?
Figure 3 presents an ICU survival tree for patients older than 70 years that was obtained by applying recursive partitioning to patients admitted to European ICUs (n=849). The classification tree comprises two main risk factor branches that include different subgroups of patients: (1) The right branch includes a high risk subgroup (survival less than 30%) of patients older than 70 years who were characterized by two events that occurred during mechanical ventilation: acute renal failure and shock; (2) The left branch of the tree is made up of patients without acute renal failure in whom survival is determined by severity at ICU admission, SAPS II score at admission and the development of hypoxemia (defined as a ratio of PaO2:FIO2 <150) over the course of the mechanical ventilation. Thus, patients with a high severity of illness (SAPS II >47) had a survival around 60%, whereas survival of patients older than 70 years with a mild severity of illness (SAPS II ≤47) was conditioned by the development of severe hypoxemia (survival of patients with severe hypoxemia was 45% versus 84% for patients without it).
Table 4 contains odds ratio estimates for each of the terminal subsets represented in the classification tree. For these calculations, the terminal subset at the extreme right was considered the reference group because it was associated with the lowest survival. Validation of the model obtained with European patients showed that the survival of risk factor subgroups was similar in USA-Canada and Latin-America. (Chi-square Hosmer-Lemeshow’s test <0.001, p=1.0)
Discussion
The main findings from this study are: we have identified an age cut-off point that is associated with worse outcome in mechanically ventilated patients; we have identified the variables that are associated with poor outcome in older patients; older patients outcome is independent of the geographical area and older patients do not consume more resources than younger patients.
The analysis of this large cohort of mechanically ventilated patients has shown 70 years as the best threshold for analyzing future cohorts and interventions in older patients requiring mechanical ventilation. While recent investigators have used that cut-off age [15], many other investigators have used other ages [14, 16, 17, 21]. An age threshold has not been previously established in a rigorous manner. Nearly half of the patients over 70 years survived until hospital discharge and rates did not differ according to geographical area after adjustment for demographic covariates and other risk factors. In keeping with several other reports, patients older than 70 years had similar intensity of care in comparison to their younger counterparts, as estimated by parameters of mechanical ventilation and length of stay. This study supports conclusions of recent publications that age alone is not a sufficient reason to withhold mechanical ventilation [9, 15], yet age should clearly be factored into “other accompanying risk factors” when estimating prognosis and attempting to make the best medical decisions for patients suffering from respiratory failure.
The current report showed that the most important factors independently associated with the highest risk of death among patients over 70 years were co-existent acute renal failure, shock and limited functional status. This observation adds considerably to important findings from recent studies of older patients with respiratory failure. In a smaller investigation restricted to medical ICU patients [9], no differences in respiratory recovery or mortality were found between younger and older patients using cut-off points of 75 years of age (the cut-off point proposed by the American Geriatric Society) and 85 years of age. The ARDS network investigators recently analyzed the effect of age on the outcome of acute lung injury [15]. They took age as a binary category and decided a priori to compare the data of patients younger and older than 70 years. In the ARDS network study, patients older than 70 years were able to oxygenate adequately and to breathe spontaneously for 2 h without ventilator assistance at a similar time point to younger patients. Passing a trial of spontaneous breathing is generally considered to indicate that a patient is ready to be removed from mechanical ventilation [22]. Despite both older and younger patients being able to breathe spontaneously for 2 h, however, the older patients had inferior outcomes, including higher reintubation rates, longer ICU and hospital stays, and lower survival rates at 28 days. In future investigations of respiratory failure in the older patient, it may be profitable to focus on unique aspects of their illness or management, such as non-pulmonary organ dysfunction or age-specific decisions related to weaning from the ventilator, which could then be targeted to improve ultimate outcome.
Several limitations of this study should be discussed. First, the data were obtained during a single month in 1998, which could pose temporal limitations on the applicability of this data set. On the other hand, the large size, international scope and variety of patients serve greatly to strengthen the importance of the work. A second limitation that might limit the generalization of our conclusions could be the inclusion of patients from countries with different economic and cultural structures. For this reason, a model for Europe was first developed and then it was shown to have achieved goodness-of-fit when the model was applied to populations from USA-Canada and Latin-America. Importantly, the development of a clinical prediction rule from the recursive partitioning trees must be prospectively studied and validated. While these data will be very important for the design of future studies in the most rapidly expanding segment of the world’s population, we believe it would be premature to apply these data to individual patients at this time. Further, other factors may have played a role in the outcomes of this cohort, such as varying thresholds for initiating mechanical ventilation according to patient age or country of enrollment and differences in rates of do-not-resuscitate orders or withdrawal of life support; this study was not designed to investigate any of these factors. Lastly, the risk of a pre-admission or pre-ventilation bias was not evaluated, thus this study may have selected a subgroup of good-prognosis elderly patients. All these important variables will have to be tracked in future studies.
It is clear that the patients over 70 years of age have significantly lower survival than younger patients, but in half of these patients the survival was higher than 60% with a similar resource utilization. In conclusion, utilization of mechanical ventilation should be considered on the basis of the patient’s underlying condition and not solely on the basis of age.
References
Jakob SM, Rothen HU (1997) Intensive care 1980–1995. Change in patients’ characteristics, nursing workload and outcome. Intensive Care Med 23:1165–1170
Hobbs F, Damon BL, Taeuber CM (1996) Sixty-five plus in United States. Bureau of The Census. Department of Commerce, Economics and Statistics Administration. Washington, DC, USA
Leaf A (1977) Medicine and the aged. N Engl J Med 297:887–890
Sage WM, Hurst CR, Silverman JF, Bortz NM (1987). Intensive care for elderly: outcome of elective and nonelective admissions. J Am Geriatric Soc 35:312–318
Baltussen R, Leidl R, Ament A (1996) The impact of age on cost-effectiveness ratios and its control in decision making. Health Econ 5:227–239
Hamel MB, Phillips RS, Teno JM, Lynn J, Galanos AN, Davis RB, Connors AF Jr, Oye RK, Desbiens N, Reding DJ, Goldman L (1996) Seriously ill hospitalized adults: do we spend less on older patients? J Am Geriatric Soc 44:1043–1048
Pesau B, Falger S, Berger E, Weimann J, Schuster E, Leithner C, Frass M (1992) Influence of age on outcome of mechanically ventilated patients in an intensive care unit. Crit Care Med 20:489–492
Angus DC, Kelley MA, Schmitz RJ, White A, Popovich J Jr, Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS) (2000) Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population?. JAMA 284:2762–2770
Ely EW, Evans GW, Haponik EF (1999) Mechanical ventilation in a cohort of elderly patients admitted to an intensive care unit. Ann Intern Med 131:96–104
Elpern EH, Larson R, Douglass P, Rosen RL, Bone RC (1989) Long-term outcomes for elderly survivors of prolonged ventilator assistance. Chest 96:1120–1124
Cohen IL, Lambrinos J (1995) Investigating the impact of age on outcome of mechanically ventilation using a population of 41,848 patients from a statewide database. Chest 107:1673–1680
Kurek CJ, Cohen IL, Lambrinos J, Minatoya K, Booth FV, Chalfin DB (1997) Clinical and economic outcome of patients undergoing tracheostomy for prolonged mechanical ventilation in New York state during 1993: analysis of 6,353 cases under diagnosis-related group 483. Crit Care Med 25:983–988
Stauffer JL, Fayter NA, Graves B, Cromb M, Lynch JC, Goebel P (1993) Survival following mechanical ventilation for acute respiratory failure in adult men. Chest 104:1222–1229
Tran DD, Groeneveld AB, van der Meulen J, Nauta JJ, Strack van Schijndel RJ, Thijs LG (1990) Age, chronic disease, sepsis, organ system failure and mortality in a medical intensive care unit. Crit Care Med 18:474–479
Ely EW, Wheeler AP, Thompson BT, Ancukiewicz M, Steinberg KP, Bernard GR for the Acute Respiratory Distress Syndrome Network (2002) Recovery rate and prognosis in older persons who develop acute lung injury and the acute respiratory distress syndrome. Ann Intern Med 136:25–36
Swinburne AJ, Fedullo AJ, Bixby K, Lee DK, Wahl GW (1993) Respiratory failure in the elderly. Analysis of outcome after treatment with mechanical ventilation. Arch Intern Med 153:1657–1662
Cohen IL, Lambrinos J, Fein JA (1993) Mechanical ventilation for the elderly patient in intensive care: incremental charges and benefits. JAMA 269:1025–1029
Giugliano RP, Camargo CA Jr, Lloyd-Jones DM, Zagrodsky JD, Alexis JD, Eagle KA, Fuster V, O’Donnell CJ (1998) Elderly patients receive less aggressive medical and invasive management of unstable angina. Arch Intern Med 158:1113–1120
Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart TE, Benito S, Epstein SK, Apezteguia C, Nightingale P, Arroliga AC, Tobin MJ, Mechanical Ventilation International Study Group (2002) Characteristics and outcomes in adult patients receiving mechanical ventilation. JAMA 287:345–355
Ciampi A, Lawless JF, McKinney SM, Singhal K (1988). Regression and recursive partition strategies in the analysis of medical survival data. J Clin Epidemiol 41:737–748
Steiner T, Mendoza G, De Georgia M, Schellinger P, Holle R, Hacke W (1997) Prognosis of stroke patients requiring mechanical ventilation in a neurological critical care unit. Stroke 28:711–715
Ely EW, Baker AM, Dunagan DP, Burke HL, Smith AC, Kelly PT, Johnson MM, Browder RW, Bowton DL, Haponik EF (1996) Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med 335:1864–1869
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors wrote this paper on behalf of the Mechanical Ventilation International Study Group, whose members are listed in the electronic supplementary material.
Supported by grant 98/0233 from the Fondo de Investigación Sanitaria, by the Red GIRA (G03/063 from the Fondo de Investigaciones Sanitarias), by the Red Respira (C03/11 from the Fondo de Investigaciones Sanitarias) and Merit Review Grant from Veterans Administration Research Service.
Dr. Ely is funded by the Paul Beeson Faculty Scholar Award for Study of Aging and the National Institute of Aging (#AG01023–01A1)
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Esteban, A., Anzueto, A., Frutos-Vivar, F. et al. Outcome of older patients receiving mechanical ventilation. Intensive Care Med 30, 639–646 (2004). https://doi.org/10.1007/s00134-004-2160-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2160-5