Abstract
Aims/hypothesis
We aimed to investigate the impact of maternal gestational weight gain (GWG) during dietary treatment on fetal growth in pregnancies complicated by gestational diabetes (GDM).
Methods
This was a retrospective cohort study of 382 women consecutively diagnosed with GDM before 34 weeks’ gestation with live singleton births in our centre (Center for Pregnant Women with Diabetes, Rigshospitalet, Copenhagen, Denmark) between 2011 and 2017. The women were stratified into three groups according to restricted (53%), appropriate (16%) and excessive (31%) weekly GWG during dietary treatment (using the Institute of Medicine guidelines) to estimate compliance with an energy-restricted ‘diabetes diet’ (6000 kJ/day [1434 kcal/day], with approximately 50% of energy intake coming from carbohydrates with a low glycaemic index, and a carbohydrate intake of 175 g/day). Insulin therapy was initiated if necessary, according to local clinical guidelines.
Results
Glucose tolerance, HbA1c, weekly GWG before dietary treatment (difference between weight at GDM diagnosis and pre-pregnancy weight, divided by the number of weeks) and SD score for fetal abdominal circumference were comparable across the three groups at diagnosis of GDM at 276 ± 51 weeks (gestation time is given as weeksdays). The women were followed for 100 ± 51 weeks, during which 54% received supplementary insulin therapy and the average (mean) GWG during dietary treatment was 0 kg, 3 kg and 5 kg in the three groups, respectively. Excessive weekly GWG during dietary treatment, reflecting poor dietary adherence was associated with increasing HbA1c (p = 0.014) from diagnosis of GDM to late pregnancy and infants with a birthweight-SD score of 0.59 ± 1.6. In contrast, restricted weekly GWG during dietary treatment, reflecting strict dietary adherence, was associated with decreasing HbA1c (p = 0.001) from diagnosis of GDM to late pregnancy and infants with a birthweight-SD score of 0.15 ± 1.1, without increased prevalence of infants born small for gestational age. Excessive GWG during dietary treatment and late-pregnancy HbA1c were identified as potentially modifiable clinical predictors of infant birthweight-SD score (p = 0.02 for both variables) after correction for confounders.
Conclusions/interpretation
Restricted GWG during dietary treatment was associated with healthier fetal growth in women with GDM. GWG during dietary treatment and late-pregnancy HbA1c were identified as potentially modifiable clinical predictors of infant birthweight-SD score.
Similar content being viewed by others

Introduction
Gestational diabetes mellitus (GDM) is associated with an increased risk of delivery of large-for-gestational age (LGA) infants and other adverse pregnancy outcomes affecting both mother and offspring in the short term [1,2,3]. Furthermore, increased long-term risks of childhood obesity and type 2 diabetes are seen among the offspring of GDM mothers [4,5,6]. There is a continuous positive association between maternal hyperglycaemia and adverse pregnancy outcomes, including fetal overgrowth [7, 8].
In individuals with GDM, dietary treatment is primarily designed to improve glycaemic control. Two large randomised controlled trials [9, 10] have shown that intensive treatment of maternal hyperglycaemia during pregnancy with diet (and insulin if necessary) is crucial for healthy fetal growth. Moreover, dietary treatment of GDM was found to decrease the risk of pregnancy complications, including excessive fetal growth, without increasing rates of infants born small-for-gestational age (SGA) [2, 3, 9,10,11].
A previous study from our centre (Center for Pregnant Women with Diabetes, Rigshospitalet, Copenhagen, Denmark), including 148 women with GDM, found that women with GDM who attained the goal for HbA1c before delivery had healthier gestational weight gain (GWG) than women who failed to achieve this goal [12]. Observational studies in women with pregestational diabetes and GDM have found that excessive maternal GWG increases the risk of adverse pregnancy outcomes, including fetal overgrowth [11, 13,14,15], and that restricted maternal GWG is associated with a healthier infant birthweight [16]. However, these studies do not evaluate the effect of intervention with dietary treatment after the diagnosis of GDM, reporting only total GWG throughout pregnancy (GWG-total). From a clinical perspective, we believe that women with GDM and their offspring are likely to benefit from restricted GWG via dietary treatment, and its impact on pregnancy, therefore, needs to be explored. Studies in healthy women have shown an increased risk of SGA infants [17, 18] and preterm delivery [19] with restricted GWG. Thus, restricted and potentially insufficient energy intake in women with GDM might result in excess SGA. The aim of this retrospective cohort study was to investigate the impact of maternal GWG during dietary treatment on fetal growth in pregnancies complicated by GDM.
Methods
Study population
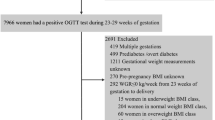
All women diagnosed with GDM before 34 weeks of gestation and followed at the Center for Pregnant Women with Diabetes, Rigshospitalet, Copenhagen, Denmark from January 2011 to March 2017 were identified for use in this study. GDM was diagnosed using Danish criteria (i.e. a 75 g OGTT with a 2 h glucose value ≥9.0 mmol/l in venous plasma or capillary whole blood) [20]. In women whose GDM was diagnosed before 20 weeks’ gestation, only those with an HbA1c ≤48 mmol/mol (≤6.5%) were included, to avoid including women with undiagnosed pre-existing diabetes. Risk-factor-based screening for GDM was applied according to national guidelines [20]. Only singleton pregnancies with live births after 22 weeks were included. If a woman had more than one pregnancy in the study period, only the first pregnancy was included. Of the 460 women who met these criteria, 62 were excluded due to incomplete maternal or offspring data, and 16 were excluded because of concomitant maternal disease (inflammatory bowel disease, severe heart disease, pulmonary embolus, previous cancer or other concurrent severe illness). Among the remaining 382 women, 183 (48%) were unselected from a local uptake area (i.e. a geographically well-defined area where all pregnant women were referred to the antenatal clinic used in this study) and 195 (51%) were selectively referred to our center from other hospitals shortly after GDM diagnosis for evaluation for possible initiation of supplementary insulin treatment, which was usually initiated during the first visit to our clinic. Data on uptake area were missing for four women. The median diagnostic 2 h glucose value was 11.5 mmol/l (range 9.0–22.7 mmol/l) vs 9.6 mmol/l (9.0–15.4 mmol/l) in referred and local women, respectively. The women who were referred, therefore, represented those with the relatively most disturbed glucose metabolism.
The Danish Data Protection Agency (3-3013-1904/1/) approved the protocol. From 2015 to 2017, informed consent was obtained from all the participating women. For the women included before 2015, we obtained permission from the Danish Health Authority to perform the study without informed consent.
Routine diabetes and pregnancy care
Shortly after the diagnosis of GDM, all women received 1 h of individualised dietary consultation with a specialised dietitian at our centre. The cornerstone of the dietary intervention was an energy-restricted diet in line with Danish national guidelines on a diet for diabetes. This contained approximately 6000 kJ/day (1434 kcal/day), of which approximately 50% of energy intake was based on carbohydrates. The diet was designed to ensure sufficient intake of minerals, vitamins, carbohydrates (175 g/day) and proteins. Supplementation with iron and vitamin D was given according to national Danish recommendations. Physical activity for at least 30 min/day was recommended. The women were informed about the Copenhagen recommendations for weekly maternal GWG in late pregnancy, based on their pre-pregnancy BMI, independent of their GWG before GDM diagnosis: 400 g/week for normal-weight (BMI <25 kg/m2), 300 g/week for overweight (BMI 25–30 kg/m2) and 200 g/week, for obese (BMI >30 kg/m2) women [21].
Throughout pregnancy, the participants were advised to self-monitor their plasma glucose levels before and 90 min after each main meal and at bedtime, in line with national guidelines. The goals for self-monitored plasma glucose levels were 4.0–6.0 mmol/l before and 4.0–8.0 mmol/l after each of the three main meals. This was measured daily in the first week after diagnosis and on at least 2 days/week, thereafter, in individuals undergoing diet treatment only. In addition, an HbA1c of 38 mmol/mol (<5.6%) in late pregnancy was set as a treatment goal [22]. HbA1c was measured using an International Federation of Clinical Chemistry (IFCC)-aligned latex immune-agglutination inhibition method [13] at diagnosis of GDM and then every 2–4 weeks, until around 37 weeks of gestation. If HbA1c values were above the target, an intensified focus was placed on self-monitored plasma glucose measurements, aiming to decrease them to the target value. All participants were offered frequent telephone contact with a specialised nurse.
Insulin treatment was initiated in addition to dietary treatment if at least two plasma glucose values exceeded the goal within 14 days of treatment with diet and physical activity. In the outpatient setting, a specialised nurse initiated insulin treatment with an initial dose of 0.3 U/kg human premixed (Novomix 30, NovoNordisk, Bagsværd, Denmark) insulin divided into two daily doses. This was chosen over basal bolus therapy to improve compliance, and we have previously published excellent results using this strategy [12]. The insulin dose was titrated via frequent telephone contact with a specialised nurse during the first 14 days and, thereafter, by contact with a diabetologist every 2–4 weeks. If the treatment goal was not met, treatment could be changed to basal bolus therapy. Episodes of hypoglycaemia were not registered in this study. Delivery was routinely planned at 40–41 weeks in women treated with diet only, and at 39–40 weeks in cases where insulin treatment had been added.
Data collection
Data on mothers, infants and pregnancy outcomes and complications were obtained from the local quality assessment database, Clinical Measure System (Region H, Copenhagen, Denmark). At diagnosis of GDM (or at referral to our centre shortly after diagnosis of GDM), the following variables were recorded: age, ethnicity, parity, smoking, self-reported pre-pregnancy weight and height, and OGTT results. HbA1c and weight were recorded at diagnosis of GDM and in late pregnancy. If relevant, insulin type and dose during pregnancy were recorded. The following data on perinatal outcomes were recorded: induction of labour, delivery mode, whether delivery was preterm, Apgar scores <7 at 5 min, respiratory distress, jaundice, admission to the neonatal intensive care unit (NICU), gestational age at delivery, and sex and birthweight of the offspring. Gestation time is presented here as weeksdays.
The antenatal fetal ultrasound examinations performed at diagnosis of GDM (mean ± SD; 291 ± 25 weeks) and in late pregnancy (370 ± 13 weeks) were recorded using the local ultrasound software system (Astraia, Munich, Germany). Results were not included in the analyses if the women had their first ultrasound examination after 34 weeks of gestation (n = 3), if the interval between the examinations was less than 14 days (n = 2) or if the examinations were missing (n = 1). For all ultrasound measurements, we recorded the actual measurement and the SD score (commonly referred to as the z score). Gestational age, SD score for fetal head circumference (HC) and SD score for fetal AC were recorded from the ultrasound scans [23].
Definitions of maternal GWG
GWG-total was defined as the difference between the last recorded maternal weight in pregnancy and the self-reported pre-pregnancy weight. Body weight was measured with light clothes, without shoes, on the same validated scale in our clinic, and given in kg to one decimal place. The last measurement was performed at 37 weeks, approximately 10 days before delivery. Weekly maternal GWG before initiation of dietary treatment was defined as the difference between the weight immediately before initiation of dietary treatment at diagnosis of GDM and the self-reported pre-pregnancy weight, divided by the number of weeks between these measurements. Weekly maternal GWG during dietary treatment was defined as the difference between the last recorded maternal weight before delivery and the weight at diagnosis of GDM divided by the number of weeks between these.
Stratification of women according to GWG during dietary treatment
Pre-pregnancy BMI was calculated based on measured or self-reported height and self-reported weight. The women were categorised as underweight (BMI <18.5 kg/m2, n = 9), normal weight (BMI 18.5–24.9 kg/m2, n = 112), overweight (BMI 25–30 kg/m2, n = 122) or obese (BMI >30 kg/m2, n = 139). Based on their pre-pregnancy BMI and the Institute of Medicine (IOM) guidelines for weekly maternal GWG during the second and third trimesters [24], the women were stratified into three groups: ‘restricted’ if GWG with dietary treatment was 440, <350, <230 and <170 g/week for each BMI category, respectively (this reflected strict dietary adherence); ‘appropriate’ if GWG with dietary treatment was within 440–580, 350–500, 230–330 and 170–270 g/week for each BMI category, respectively; and ‘excessive’ if GWG with dietary treatment was >580, >500, >330 and >270 g/week for each BMI category, respectively (reflecting poor dietary adherence) [24].
Definitions of maternal and neonatal outcomes
Preterm delivery was defined as birth before 37 completed gestational weeks (259 days). The primary outcome for fetal growth was infant birthweight-SD score, which was defined as deviation from the mean of a Nordic population, adjusted for gestational age and sex [25]. Accordingly, SGA was defined as birthweight below the 10th percentile (SD score less than −1.28), and LGA was defined as birthweight above the 90th percentile (SD score above1.28).
Statistics
All continuous variables are presented as mean (± SD) except glucose values from the diagnostic OGTTs, which, owing to skewed distribution, are presented as median and range. Categorical variables are presented as numbers (%). Unpaired one-way ANOVA and Kruskal–Wallis tests were used for parametric and non-parametric comparisons of continuous variables, respectively, while the χ2 test was used for categorical variables, when comparing women with restricted, appropriate or excessive GWG during dietary treatment. If a difference was found using these tests, pairwise comparisons between women with restricted, appropriate and excessive GWG during dietary treatment were performed using an unpaired t test, Mann–Whitney test or χ2 test as appropriate, followed by correction for multiple testing using the Bonferroni method. A paired t test was used only to compare changes from diagnosis of GDM to the last visit. Univariate linear regression analysis was performed to explore the association between the SD score for infant birthweight and each of the following variables: maternal age (years); parity ≥1 (yes/no); ethnicity (Nordic/non-Nordic); smoking (yes/no); referral from other hospitals (yes/no); height (cm); pre-pregnancy BMI (kg/m2); 2 h OGTT glucose concentration (mmol/l); HbA1c at diagnosis of GDM and in late pregnancy (mmol/mol); insulin treatment (yes/no); GWG during dietary treatment (g/week); excessive GWG during dietary treatment (yes/no); GWG-total (kg) and SD score for ultrasound-based fetal AC at GDM diagnosis. Multivariate linear regression analysis was performed to identify independent predictors of SD score for infant birthweight, including variables with p < 0.1 in the univariate analyses. Only pre-pregnancy BMI, HbA1c in late pregnancy and excessive GWG during dietary treatment were included in the multivariate regression analyses, due to the expected close associations between the following variables: (1) height and pre-pregnancy BMI; (2) HbA1c at GDM diagnosis and in late pregnancy; and (3) GWG-total, weekly GWG during dietary treatment and excessive GWG during dietary treatment. SD score for fetal AC was also not included in the multivariate regression analysis owing to its strong correlation with SD score for infant birthweight .
The statistical analyses were performed using IBM SPSS statistics 22 (SPSS, Chicago, IL, USA). Differences were considered statistically significant at a two-sided p value <0.05, with correction for multiple comparisons, as noted above.
Results
In total, 382 women diagnosed with GDM at 276 ± 51 gestational weeks were stratified into three GWG groups according to weekly GWG during dietary treatment, with 53% having restricted, 16% appropriate and 31% excessive GWG during the 100 ± 51 weeks of dietary treatment (Table 1). At diagnosis of GDM, the three GWG during dietary treatment (GWG-on-diet) groups were comparable regarding 2 h OGTT glucose, weekly GWG before dietary treatment, HbA1c and SD score for fetal AC (Tables 1 and 2). Pre-pregnancy BMI was slightly higher among women in the excessive GWG-on-diet group (p = 0.001; Table 1).
Maternal outcome
During the approximately 10 weeks from diagnosis of GDM to late pregnancy, the average (mean) weight gain in the restricted, appropriate and excessive GWG-on-diet groups was 0 kg, 3 kg and 5 kg, respectively (Table 1). The majority of women in the restricted GWG-on-diet group, held a stable weight during the intervention. Only 15 women (7%) in this group had a weight loss ≥500 g/week. In late pregnancy, HbA1c levels differed across the groups (p = 0.009; Table 1), with the highest values in women in the excessive GWG-on-diet group (Table 1). A decrease in HbA1c was seen for women in the restricted GWG-on-diet group (p = 0.001), while an increase in HbA1c after dietary intervention was observed for women in the excessive GWG-on-diet group (p = 0.014). Vaginal delivery was less prevalent in women in the excessive GWG-on-diet group (p = 0.001), with more emergency Caesarean sections being reported in this group (Table 2).
Women requiring supplementary insulin treatment (54%) were characterised by higher pre-pregnancy BMI and HbA1c at diagnosis of GDM and a higher weekly GWG during dietary treatment compared with women treated with diet alone (280 ± 412 g/week vs 116 ± 378 g/week; p < 0.001; Table 3).
Fetal growth before GDM diagnosis and during dietary treatment
Ultrasound examinations were available for 376 (98%) women (Table 2). The SD score for fetal HC was close to zero and remained stable from GDM diagnosis to late pregnancy, with no differences observed across the three GWG-on-diet groups. At diagnosis of GDM, the fetal AC-SD-score was approximately +0.5, with 23% of fetuses having an AC-SD score above the 90th percentile in all three groups. The SD score for fetal AC increased in all three GWG-on-diet groups during the intervention, with 43% of fetuses having an AC-SD score above the 90th percentile in late pregnancy. The increase was highest among women in the excessive GWG-on-diet group. Univariate logistic regression analyses identified 2 h OGTT glucose, HbA1c at GDM diagnosis, weekly GWG before dietary treatment and referral from other hospitals as being positively associated with fetal AC-SD score above the 90th percentile at GDM diagnosis (see electronic supplementary material [ESM] Table 1).
Infant birthweight-SD score, LGA and SGA
Infant birthweight-SD score was higher for women in the excessive GWG-on-diet group, reflecting poor dietary adherence, compared with women in the restricted GWG-on-diet group (0.59 ± 1.6 vs 0.15 ± 1.1; p = 0.008; Table 2). No difference was found in the remaining pairwise comparisons of infant birthweight-SD score with women in the restricted and appropriate GWG-on-diet groups, or the appropriate and excessive GWG-on-diet groups (Table 2). The prevalence of SGA and LGA was comparable across the three GWG-on-diet groups (Table 2). Women treated with diet and supplementary insulin delivered infants with higher birthweight-SD scores than women treated with diet only (Table 3). Among the unselected women from the local uptake area, 32% were treated with diet and supplementary insulin; 16% of infants born to these insulin-treated women were born LGA and 10% were born SGA.
Clinical predictors of birthweight-SD score
Univariate linear regression analyses identified weekly GWG during dietary treatment, GWG-total, excessive GWG during dietary treatment and HbA1c at diagnosis of GDM and in late pregnancy as potentially modifiable clinical predictors of infant birthweight-SD score (Table 4). Fetal AC-SD score at GDM diagnosis was strongly associated with infant birthweight-SD score (p < 0.001; Table 4).
In the multivariate linear regression analysis, excessive GWG during dietary treatment and HbA1c in late pregnancy were identified as potentially modifiable clinical predictors of infant birthweight-SD score (p = 0.02 for both variables) after correction for parity, uptake area, pre-pregnancy BMI and supplementary treatment with insulin. Replacing the categorical variable ‘excessive GWG during dietary treatment’ with the continuous variable ‘weekly GWG during dietary treatment’ resulted in similar clinical predictors. Maternal GWG during dietary treatment was still identified as a clinical predictor of infant birthweight-SD score when the fetal AC-SD score at GDM diagnosis was included in the analysis. For the subgroup of women treated with supplementary insulin (n = 204), weekly GWG during dietary treatment and HbA1c in late pregnancy remained as potentially modifiable clinical predictors for infant birthweight-SD score in univariate linear regression analyses (data not shown).
Discussion
In this cohort study, women with GDM and restricted GWG during dietary treatment (considered a marker of dietary adherence) showed a reduced risk of fetal overgrowth without any increased risk of fetal growth restriction. Excessive GWG during dietary treatment and HbA1c in late pregnancy were potentially modifiable clinical predictors of birthweight-SD score.
To our knowledge, this is the first observational study addressing the association of maternal GWG during dietary treatment with fetal growth that includes fetal growth data from of the point of GDM diagnosis. The main goal of dietary treatment has traditionally been to reduce maternal hyperglycaemia during pregnancy [9, 10] to reduce the fetal glycaemic burden, rather than focusing specifically on restricting GWG. It is well known that fetal growth is positively associated with maternal GWG, and that healthy women with excessive GWG run a higher risk of excessive fetal growth [26,27,28]. Previous studies have also shown an association between excessive maternal GWG and the risk of delivering an LGA infant in women with GDM [11, 14, 15]. In women with type 2 diabetes, restricted maternal GWG was associated with a healthier infant birthweight [16]. The studies in women with GDM [11, 14, 15] assessed maternal GWG over the whole course of pregnancy without distinguishing between GWG before and after the onset of dietary intervention. Therefore, they were not able to explore the effect of dietary treatment and GWG after GDM diagnosis on fetal growth and pregnancy outcome. Maternal blood glucose levels during pregnancy are known to have a major impact on fetal growth, and the continuous association between maternal hyperglycaemia and adverse pregnancy outcomes for women with GDM has been demonstrated in the Hyperglycemia and Adverse Pregnancy Outcome [HAPO] study [7]. In our study, adherence to the strict diet intervention during treatment for GDM varied between the participants and, hence, we categorised participants according to restricted, appropriate and excessive GWG during dietary treatment. To our knowledge, we are the first to demonstrate that restricted GWG during dietary treatment is associated with both a small decline in HbA1c and a reduced risk of fetal overgrowth.
Restricted maternal GWG is associated with an increase in the prevalence of SGA infants in healthy women [17,18,19, 29], but our study findings suggest that this might be different in women with GDM. A rate of 10% for infants born SGA, as observed in this study, is relatively high for women with disturbed glucose tolerance. This relative infant birthweight was calculated based on Nordic background population data without correction for ethnicity. Around half of the women in our study were of non-Nordic origin, mostly from populations with a lower average (mean) birthweight than Danish women of Nordic origin, which may have affected the SGA rate in our study. However, it is reassuring that we did not find an increased risk of SGA infants among women with restricted GWG during dietary treatment, compared with the background population. However, the number of women in this group of included women is relatively small, making it difficult to draw solid conclusions. Furthermore, the fetal HC-SD score, reflecting the size of the cerebrum, was unaffected by maternal GWG during dietary treatment, with stable and comparable SD scores for fetal HC in all three GWG-on-diet groups. These findings suggest that the fetuses of women with GDM may be protected from growth restriction despite the restricted maternal energy intake compared with the fetuses of healthy women. Another possible reason for a low risk of fetal growth restriction in women with GDM in the restricted GWG during dietary treatment group might be that the women in our study were treated with a diet sufficient in protein, minerals and vitamins. This may be in contrast to epidemiological studies, where restricted GWG may be related to insufficient intake of energy, protein, minerals and vitamins, inducing a higher risk of SGA infants. Based on our findings, restriction of GWG during dietary treatment to the level observed in the present study may be beneficial in preventing fetal overgrowth without increasing the risk of fetal growth restriction during pregnancy in women with GDM. Unfortunately, infant HC and AC and the long-term health of the offspring were not recorded but could have added relevant information to the study.
Excessive GWG during dietary treatment and HbA1c in late pregnancy were identified as potentially modifiable clinical predictors of infant birthweight-SD score independent of treatment with insulin. In accordance with a previous study from our group [12], the present study showed that women who were on insulin, as well as dietary treatment, gained more weight than women on dietary treatment alone, but on average, they still had a lower mean weekly GWG than earlier in pregnancy where dietary intervention and supplementary insulin treatment had not yet been given. Whether initiation of insulin treatment in our study was related to insufficient dietary adherence or whether the insulin treatment itself induced increased GWG merits discussion. The women who had insulin treatment initiated in addition to dietary treatment were mainly characterised by poorer glycaemic control but comparable GWG prior to diagnosis of GDM as compared with the women treated with diet alone. In contrast, Egan et al [15] found a lower GWG in women with GDM treated with diet and insulin when compared with women treated with diet alone.
In our study, women treated with diet and supplementary insulin showed reductions in HbA1c from diagnosis of GDM to late pregnancy but did not achieve the goal for HbA1c before delivery or appropriate fetal growth. Clinical guidelines with a focus on the importance of fast and appropriate insulin initiation and increment in pregnancy complicated by GDM are, therefore, probably needed. Excessive fetal growth can be measured by ultrasound at diagnosis of GDM, as shown in our study and by others [8], and earlier diagnosis and treatment may reduce fetal overgrowth. Women treated with diet and supplementary insulin had higher weekly GWG than women on dietary treatment only, but the weekly GWG seems to be lower in all women after the initiation of dietary intervention regardless of insulin treatment.
Women in the excessive GWG-on-diet group showed a slight increase in HbA1c, while women in the restricted or appropriate GWG-on-diet groups showed decreased or stable HbA1c levels throughout the remainder of pregnancy. This is in accordance with a previous study from our group in which women with less strict glycaemic control gained more weight than women with strict glycaemic control [12]. HbA1c reflects the mean blood glucose level over the past 2–3 months and cannot necessarily detect the presence of glucose fluctuations, which may also have detrimental effects on fetal growth [12, 30].
In accordance with a British study [8], approximately one out of five fetuses had an AC-SD score that was above the 90th percentile. In the present study, the increase in fetal AC-SD score, birthweight SD score and prevalence of emergency Caesarean section was highest in women with excessive GWG during dietary treatment. The prevalence of LGA infants in the subgroup of unselected women from our local uptake area is comparable with the findings from a study in Ireland [15], in which the prevalence of LGA infants being born to women with diet-treated GDM was 18%, and a combination of excessive GWG-total and supplementary insulin treatment increased the risk of having an LGA infant [15].
The strengths of our study are the large cohort of women (n = 382) with fetal ultrasound data on diagnosis of GDM and in late pregnancy. Unlike previous studies, data on weekly maternal GWG were available from before and after the diagnosis of GDM, allowing us to assess the effect of an energy-restricted diet for diabetes. However, the current study is limited by retrospective data collection. Our cohort consisted of women from the local uptake area, which can be regarded as an unselected cohort, and women referred from other hospitals for evaluation for potential initiation of insulin treatment. In addition, it would have been advantageous if women were referred earlier as there was a limited window to initiate dietary treatment and titrate insulin doses for optimal therapy.
Denmark has a long-standing tradition of diagnosing GDM based on 2 h OGTT values and identifying newly developed type 2 diabetes as overt diabetes when diagnosed before 20 weeks. In this study, 32% of the women had diagnostic 2 h glucose values ≥11.1 mmol/l and all women were diagnosed after 20 weeks. Our population may differ from type 2 diabetic populations based upon the International Association of the Diabetes and Pregnancy Study Groups (IADPGS)/WHO criteria, but the majority of women would probably have been diagnosed regardless of which criteria were used. Self-reported pre-pregnancy weight was used to calculate pre-pregnancy BMI and GWG before dietary treatment, with an inevitable risk of recall bias. All women received the same dietary intervention, but as we do not have data on compliance or other variables that may influence adherence to therapy, we cannot exclude other factors that influence pregnancy outcome in affecting the results of this study. The recommended diet may have been too restrictive in underweight women since three out of nine of these women delivered SGA infants. In addition, the development of fluid retention and oedema during pregnancy, which could potentially impact GWG, was not recorded. It is reassuring that no differences regarding risk of delivering a preterm infant were found across the three GWG groups. However, sufficient micronutrient intake must be ensured, and future studies on the long-term implications of specific dietary interventions during pregnancy are needed. Unfortunately, we did not collect data on average (mean) plasma glucose values or on biochemical hypoglycaemia. Severe hypoglycaemic episodes were also not reported.
In conclusion, restricted GWG during dietary treatment was associated with healthier fetal growth in women with GDM when compared with women with excessive GWG. Excessive GWG during dietary treatment and HbA1c in late pregnancy were potentially modifiable clinical predictors of fetal growth. Focus on both appropriate weekly maternal GWG during dietary treatment and good glycaemic control in women with GDM is likely important to obtain appropriate fetal growth in women with GDM.
Contribution statement
LLK and ERM contributed to conception and design of the study and acquired the data. All authors took part in acquisition of data or analysis and interpretation of the data. LLK performed the initial draft of the article. SKN, ALS, VLN, HR, AT, HDM, PD and ERM contributed to drafting the article and revising it critically for important intellectual content. All authors gave their final approval of the version to be published. ERM is the guarantor of this work.
Data availability
Source data are available on written request to L. Kurtzhals.
Abbreviations
- AC:
-
Abdominal circumference
- GDM:
-
Gestational diabetes mellitus
- GWG:
-
Gestational weight gain
- GWG-on-diet:
-
Gestational weight gain during dietary treatment (group)
- GWG-total :
-
Gestational weight gain throughout pregnancy
- HC :
-
Head circumference
- LGA :
-
Large for gestational age
- SGA:
-
Small for gestational age
References
Ovesen PG, Jensen DM, Damm P, Rasmussen S, Kesmodel US (2015) Maternal and neonatal outcomes in pregnancies complicated by gestational diabetes. A nation-wide study. Matern Fetal Neonatal Med 28:1720–1724. https://doi.org/10.3109/14767058.2014.966677
Gonzalez-Quintero VH, Istwan NB, Rhea DJ et al (2007) The impact of glycemic control on neonatal outcome in singleton pregnancies complicated by gestational diabetes. Diabetes Care 30:467–470. https://doi.org/10.2337/dc06-1875
Langer O, Yogev Y, Most O, Xenakis EM (2005) Gestational diabetes: the consequences of not treating. Am J Obstet Gynecol 192:989–997. https://doi.org/10.1016/j.ajog.2004.11.039
Dabelea D, Mayer-Davis EJ, Lamichhane AP et al (2008) Association of intrauterine exposure to maternal diabetes and obesity with type 2 diabetes in youth: the SEARCH Case-Control Study. Diabetes Care 31:1422–1426. https://doi.org/10.2337/dc07-2417
Petitt DJ, Bennett PH, Knowler WC, Baird HR, Aleck KA (1985) Gestational diabetes mellitus and impaired glucose tolerance during pregnancy. Long-term effects on obesity and glucose tolerance in the offspring. Diabetes 34(Suppl 2):119–122. https://doi.org/10.2337/diab.34.2.S119
Clausen TD, Mathiesen ER, Hansen T et al (2008) High prevalence of type 2 diabetes and pre-diabetes in adult offspring of women with gestational diabetes mellitus or type 1 diabetes: the role of intrauterine hyperglycemia. Diabetes Care 31:340–346. https://doi.org/10.2337/dc07-1596
Metzger BE, Lowe LP, Dyer AR et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358:1991–2002. https://doi.org/10.1056/NEJMoa0707943
Sovio U, Murphy HR, Smith GC (2016) Accelerated fetal growth prior to diagnosis of gestational diabetes mellitus: a prospective cohort study of nulliparous women. Diabetes Care 39:982–987. https://doi.org/10.2337/dc16-0160
Landon MB, Spong CY, Thom E et al (2009) A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med 361:1339–1348. https://doi.org/10.1056/NEJMoa0902430
Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS (2005) Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 352:2477–2486. https://doi.org/10.1056/NEJMoa042973
Kgosidialwa O, Egan AM, Carmody L, Kirwan B, Gunning P, Dunne FP (2015) Treatment with diet and exercise for women with gestational diabetes mellitus diagnosed using IADPSG criteria. J Clin Endocrinol Metab 100:4629–4636. https://doi.org/10.1210/jc.2015-3259
Mikkelsen MR, Nielsen SB, Stage E, Mathiesen ER, Damm P (2011) High maternal HbA1c is associated with overweight in neonates. Dan Med Bull 58:A4309
Secher AL, Parellada CB, Ringholm L, Asbjornsdottir B, Damm P, Mathiesen ER (2014) Higher gestational weight gain is associated with increasing offspring birth weight independent of maternal glycemic control in women with type 1 diabetes. Diabetes Care 37:2677–2684. https://doi.org/10.2337/dc14-0896
Kim SY, Sharma AJ, Sappenfield W, Wilson HG, Salihu HM (2014) Association of maternal body mass index, excessive weight gain, and gestational diabetes mellitus with large-for-gestational-age births. Obstet Gynecol 123:737–744. https://doi.org/10.1097/AOG.0000000000000177
Egan AM, Dennedy MC, Al-Ramli W, Heerey A, Avalos G, Dunne F (2014) ATLANTIC-DIP: excessive gestational weight gain and pregnancy outcomes in women with gestational or pregestational diabetes mellitus. J Clin Endocrinol Metab 99:212–219. https://doi.org/10.1210/jc.2013-2684
Asbjornsdottir B, Rasmussen SS, Kelstrup L, Damm P, Mathiesen ER (2013) Impact of restricted maternal weight gain on fetal growth and perinatal morbidity in obese women with type 2 diabetes. Diabetes Care 36:1102–1106. https://doi.org/10.2337/dc12-1232
Nohr EA, Vaeth M, Baker JL, Sorensen T, Olsen J, Rasmussen KM (2008) Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. Am J Clin Nutr 87:1750–1759. https://doi.org/10.1093/ajcn/87.6.1750
Cogswell ME, Serdula MK, Hungerford DW, Yip R (1995) Gestational weight gain among average-weight and overweight women--what is excessive? Am J Obstet Gynecol 172:705–712. https://doi.org/10.1016/0002-9378(95)90598-7
Nohr EA, Bech BH, Vaeth M, Rasmussen KM, Henriksen TB, Olsen J (2007) Obesity, gestational weight gain and preterm birth: a study within the Danish National Birth Cohort. Paediatr Perinat Epidemiol 21:5–14. https://doi.org/10.1111/j.1365-3016.2007.00762.x
Gynaecology DSoOa (2014) Clinical guideline on gestational diabetes mellitus: screening and diagnosis [in Danish]. Available from http://gynobsguideline.dk/wp/wp-content/uploads/2013/02/GDM-Sandbjerg-2014-godkendt-2014.pdf. Accessed 30 Oct 2017
Norgaard SK, Nichum VL, Barfred C et al (2017) Use of the smartphone application “Pregnant with Diabetes”. Dan Med J 64:pii:A5417
Nielsen LR, Ekbom P, Damm P et al (2004) HbA1c levels are significantly lower in early and late pregnancy. Diabetes Care 27:1200–1201. https://doi.org/10.2337/diacare.27.5.1200
Hadlock FP, Harrist RB, Martinez-Poyer J (1991) In utero analysis of fetal growth: a sonographic weight standard. Radiology 181:129–133. https://doi.org/10.1148/radiology.181.1.1887021
Institute of Medicine (2009) Weight gain during pregnancy: reexamining the guidelines. Available from www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines/Report%20Brief%20-%20Weight%20Gain%20During%20Pregnancy.pdf. Accessed 30 Oct 2017
Marsal K, Persson PH, Larsen T, Lilja H, Selbing A, Sultan B (1996) Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr 85:843–848. https://doi.org/10.1111/j.1651-2227.1996.tb14164.x
Dietz PM, Callaghan WM, Sharma AJ (2009) High pregnancy weight gain and risk of excessive fetal growth. Am J Obstet Gynecol 201:e1–e6. https://doi.org/10.1016/j.ajog.2009.04.051
Hedderson MM, Weiss NS, Sacks DA et al (2006) Pregnancy weight gain and risk of neonatal complications: macrosomia, hypoglycemia, and hyperbilirubinemia. Obstet Gynecol 108:1153–1161. https://doi.org/10.1097/01.AOG.0000242568.75785.68
Mochhoury L, Razine R, Kasouati J, Kabiri M, Barkat A (2013) Body mass index, gestational weight gain, and obstetric complications in Moroccan population. J Pregnancy. https://doi.org/10.1155/2013/379461
Catalano PM, Mele L, Landon MB et al (2014) Inadequate weight gain in overweight and obese pregnant women: what is the effect on fetal growth? Am J Obstet Gynecol 211:e131–e137
Derr R, Garrett E, Stacy GA, Saudek CD (2003) Is HbA1c affected by glycemic instability? Diabetes Care 26:2728–2733. https://doi.org/10.2337/diacare.26.10.2728
Funding
ERM was funded by Novo Nordisk Foundation. The Novo Nordisk Foundation did not have any influence on this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that there is no duality of interest associated with this manuscript.
Electronic supplementary material
ESM Table 1
(PDF 51 kb)
Rights and permissions
About this article
Cite this article
Kurtzhals, L.L., Nørgaard, S.K., Secher, A.L. et al. The impact of restricted gestational weight gain by dietary intervention on fetal growth in women with gestational diabetes mellitus. Diabetologia 61, 2528–2538 (2018). https://doi.org/10.1007/s00125-018-4736-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4736-6