Abstract
Background
Left ventricular filling pressure (LVFP) is raised by the compromised contraction and impaired ventricular compliance in dilated hearts with systolic dysfunction. Timely recognition and staging of this condition are important for planning of the treatment strategy and making the prognosis. Two-dimensional speckle- tracking echocardiography (2D-STE) has recently enabled the quantification of left atrial (LA) myocardial deformation dynamics. In this study, echocardiographic indicators of increased LVFP and NT-pro-BNP were compared with LA strain measured by 2D-STE.
Methods
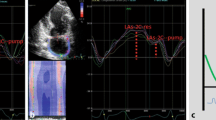
A total of 49 nonischemic dilated cardiomyopathy (DCMP) patients were included in the study. All patients underwent standard 2D echocardiography. In the 2D-STE analysis of the LA, global longitudinal LA strain during ventricular systole (GLAs-res) and strain during late diastole (GLAs-pump) were obtained. NT-pro-BNP levels were measured. The patients were divided into two groups—normal (group 1) and increased (group 2) LVFP—according to E/A ratio, E velocity, and E/E’ ratio.
Results
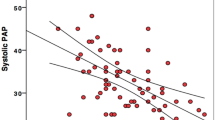
LAVi-max, LAVi-min, and NT-pro-BNP were higher in group 2, whereas LAtotalEF, LAactiveEF, GLAs-res, and GLAs-pump were lower. In univariate analysis, a good negative correlation was seen between GLAs-res vs. NT-pro-BNP, GLAs-res vs. LAVi-max, and GLAs-res vs. E/E’ ratio; a good negative correlation was present between GLAs-pump vs. NT-pro-BNP, GLAs-pump vs. LAVi-max, and GLAs-pump vs. E/E’ ratio. LAVi-max, LAactiveEF, NT-pro-BNP, GLas-res, and GLAs-pump were studied by logistic regression analysis. GLAs-res (p = 0.009, OR = 0.593, 95 % CI 0.4–0.877), NT-pro-BNP (p = 0.028, OR = 1.027, 95 % CI 1.003–1.052), and LAactiveEF (p = 0.022, OR = 0.001, 95 % CI 0.001–0.024) were found to be independent predictors of increased LVFP.
Conclusion
2D-STE-based LA function is impaired in patients with nonischemic DCMP. LA reservoir and pump function parameters together with NT-pro-BNP levels might be useful in estimating LVFP in this patient group.
Zusammenfassung
Hintergrund
Der linksventrikuläre Füllungsdruck (LVFP) ist durch die beeinträchtigte Kontraktion und gestörte ventrikuläre Compliance bei einer Herzdilatation mit systolischer Funktionsstörung erhöht. Zur Planung der Therapiestrategie und Vorhersage der Prognose sind die frühzeitige Erkennung und Klassifizierung dieser Erkrankung von Bedeutung. Durch die 2-D-Speckle-Tracking-Echokardiographie (2D-STE) ist die Quantifizierung der linksatrialen myokardialen Deformationsdynamik seit Kurzem möglich geworden. In der vorliegenden Studie wurden echokardiographische Indikatoren eines erhöhten LVFP und NT-pro-BNP („n-terminal pro brain natriuretic peptide“) mit der per 2D-STE gemessenen linksatrialen Deformierung („strain“) verglichen.
Methoden
Insgesamt wurden 49 Patienten mit nichtischämischer dilatativer Kardiomyopathie (DCMP) in die Studie aufgenommen. Bei sämtlichen Patienten erfolgte eine Standard-2-D-Echokardiographie. Mit der 2D-STE wurden die globale longitudinale linksatriale Deformierung während der Ventrikelsystole (GLAs-res) und die Deformierung während der späten Diastole (GLAs-pump) ermittelt. Auch die NT-pro-BNP-Werte wurden bestimmt. Die Patienten wurden in 2 Gruppen aufgeteilt, je nachdem, ob der LVFP gemäß E/A-Verhältnis, E-Geschwindigkeit und E/E‘-Verhältnis normal (Gruppe 1) oder erhöht (Gruppe 2) war.
Ergebnisse
In Gruppe 2 waren LAVi-max, LAVi-min und NT-pro-BNP höher, LAtotalEF, LAactiveEF, GLAs-res und GLAs-pump dagegen niedriger. In der univariaten Analyse wurde eine gute negative Korrelation zwischen GLAs-res vs. NT-pro-BNP, GLAs-res vs. LAVi-max und GLAs-res vs. E/E’-Verhältnis beobachtet, und eine gute negative Korrelation fand sich zwischen GLAs-pump vs. NT-pro-BNP, GLAs-pump vs. LAVi-max und GLAs-pump vs. E/E’-Verhältnis. LAVi-max, LAactiveEF, NT-pro-BNP, GLas-res und GLAs-pump wurden mittels logistischer Regressionsanalyse untersucht. GLAs-res (p = 0,009; OR = 0,593; 95 %-KI: 0,4–0,877), NT-pro-BNP (p = 0,028; OR = 1,027; 95 %-KI: 1,003–1,052) und LAactiveEF (p = 0,022; OR = 0,001; 95 %-KI: 0,001–0,024) stellten sich als unabhängige Prädiktoren eines erhöhten LVFP heraus.
Schlussfolgerung
Die mit der 2D-STE ermittelte linksatriale Funktion ist bei Patienten mit nichtischämischer DCMP beeinträchtigt. Die Parameter für die Reservoir- und Pumpfunktion des linken Vorhofs könnten zusammen mit den NT-pro-BNP-Werten bei der Abschätzung des LVFP in dieser Patientengruppe von Nutzen sein.


Similar content being viewed by others
References
Stevenson WG, Stevenson LW, Middlekauff HR et al (1995) Improving survival for patients with advanced heart failure: a study of 737 consecutive patients. J Am Coll Cardiol 26:1417–1423
Rihal CS, Nishimura RA, Hatle LK et al (1994) Systolic and diastolic dysfunction in patients with clinical diagnosis of dilated cardiomyopathy. Relation to symptoms and prognosis. Circulation 90:2772–2779
Skaluba SJ, Litwin SE (2004) Mechanisms of exercise intolerance: insights from tissue Doppler imaging. Circulation 109:972–977
Haskell RJ, French WI (1988) Accuracy of left atrial and pulmonary artery wedge pressure in pure mitral regurgitation in predicting ventricular end-diastolic pressure. Am J Cardiol 61:136–141
Keogh AM, Baron DW, Hikie JB (1990) Prognostic guides in patients with idiopathic or ischemic dilated cardiomyopathy for cardiac transplantation. Am J Cardiol 65:903–908
Stevenson WG, Stevenson LW, Middlekauff HR et al (1995) Improving survival for patients with advanced heart failure: a study of 737 consecutive patients. J Am Coll Cardiol 26:1417–1423
Nagueh SF, Appleton CP, Gillebert TC et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22(2):107–133
Paulus WJ, Tsche C, Sanderson JE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 28:2539–2550
Hillis GS, Moller JE, Pellikka PA et al (2004) Noninvasive estimation of left ventricular filling pressure by E/e’ is a powerful predictor of survival after acute myocardial infarction. J Am Coll Cardiol 43:360–367
Mullens W, Borowski AG, Curtin RJ et al (2009) Tissue Doppler imaging in the estimation of intracardiac filling pressure in decompensated patients with advanced systolic heart failure. Circulation 119:62–70
Bruch C, Grude M, Müller J et al (2005) Usefulness of tissue Doppler imaging for estimation of left ventricular filling pressures in patients with systolic and diastolic heart failure. Am J Cardiol 95:892–895
Lee CY, Burnett JC Jr (2007) Natriuretic peptides and therapeutic applications. Heart Fail Rev 12(2):131–142
McCullough PA, Nowak RM, McCord J et al (2002) B-type natriuretic peptide and clinical judgment in emergency diagnosis of heart failure: analysis from Breathing Not Properly (BNP) Multinational Study. Circulation 106(4):416–422
Januzzi JL Jr (2006) Natriuretic peptide testing: a window into the diagnosis and prognosis of heart failure. Cleve Clin J Med 73(2):149–152, 155–157
Lang RM, Bierig M, Devereux RB et al (2006) American Society of Echocardiography’s Nomenclature and Standards Committee; Task Force on Chamber Quantification; American College of Cardiology Echocardiography Committee; American Heart Association; European Association of Echocardiography, European Society of Cardiology. Recommendations for chamber quantification. Eur J Echocardiogr 7(2):79–108
Rudski LG, Lai WW, Afilalo J et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23(7):685–713
Kircher B, Abbott JA, Pau S et al (1991) Left atrial volume determination by biplane two-dimensional echocardiography: validation by cine computed tomography. Am Heart J 121(3 Pt 1):864–871
Kurt M, Tanboga IH, Aksakal E et al (2012) Relation of left ventricular end-diastolic pressure and N-terminal pro-brain natriuretic peptide level with left atrial deformation parameters. Eur Heart J Cardiovasc Imaging 13(6):524–530
Ohtani K, Yutani C, Nagata S et al (1995) High prevalence of atrial fibrosis in patients with dilated cardiomyopathy. J Am Coll Cardiol 25:1162–1169
Triposkiadis F, Pitsavos C, Boudoulas H et al (1994) Left atrial myopathy in idiopathic dilated cardiomyopathy. Am Heart J 128(2):308–315
Tigen K, Karaahmet T, Kirma C et al (2010) The association of functional mitral regurgitation and anemia in patients with non-ischemic dilated cardiomyopathy. Cardiol J 17(3):274–280
D’Andrea A, Caso P, Romano S et al (2009) Association between left atrial myocardial function and exercise capacity in patients with either idiopathic or ischemic dilated cardiomyopathy: a two-dimensional speckle strain study. Int J Cardiol 132(3):354–363
Conflict of interest
On behalf of all authors, the corresponding author states that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guler, A., Tigen, K., Dundar, C. et al. Left atrial deformation and nonischemic dilated cardiomyopathy. Herz 39, 251–257 (2014). https://doi.org/10.1007/s00059-013-3817-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-013-3817-z