Abstract
Aim
Nonalcoholic fatty liver disease (NAFLD) is the most common liver disorder which is reported as the hepatic manifestation of metabolic syndrome with an increased risk of cardiovascular events. Patients with NAFLD are also at risk of future cardiac events independently of metabolic syndrome. The aim of this study was to examine serum concentrations of heart type fatty acid binding protein (H-FABP) in NAFLD and to investigate its correlations with metabolic parameters and subclinical atherosclerosis.
Patients and methods
A total of 34 patients with NAFLD and 35 healthy subjects were enrolled in the study. NAFLD patients had elevated liver enzymes and steatosis graded on ultrasonography. Healthy subjects had normal liver enzymes and no steatosis on ultrasonography. H-FABP levels were measured using an enzyme linked immunosorbent assay (ELISA) method and correlations with metabolic parameters and subclinical atherosclerosis were examined. Subclinical atherosclerosis was determined with carotid artery intima–media thickness (CIMT) which was measured by high resolution B mode ultrasonography.
Results
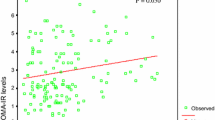
H-FABP levels were elevated in patients with NAFLD (16.3 ± 4.0 ng/ml) when compared with healthy controls (13.8 ± 2.1 ng/ml; p < 0.001). NAFLD patients had significantly higher CIMT than the controls had (0.64 ± 0.17 mm vs. 0.43 ± 0.14 mm, p = 0.009). The H-FABP concentrations were significantly positively correlated with body mass index (r = 0.255, p = 0.042), fasting blood glucose level (r = 0.300, p = 0.013), CIMT (r = 0.335, p = 0.043), and homeostasis model assessment-estimated insulin resistance (HOMA-IR; r = 0.156, p = 0.306). In multiple linear regression analysis, H-FABP levels were only independently associated with CIMT (p = 0.04)
Conclusion
Serum H-FABP concentrations increase in patients with NAFLD. Our results may not only suggest that H-FABP is a marker of subclinical myocardial damage in patients with NAFLD but also of subclinical atherosclerosis, independent of metabolic syndrome and cardiac risk factors.
Zusammenfassung
Ziel
Die nichtalkoholbedingte Steatosis hepatis (NAFLD) ist die häufigste Lebererkrankung, die als hepatische Manifestation eines metabolischen Syndroms mit erhöhtem Risiko für kardiovaskuläre Ereignisse angegeben wird. Auch unabhängig von einem metabolischen Syndrom haben NAFLD-Patienten ein erhöhtes Risiko für kardiale Ereignisse. Ziel der Studie war es, die Serumkonzentrationen von H-FABP (herzspezifisches fettsäurebindendes Protein, „heart type fatty acid binding protein“) bei NAFLD-Patienten zu bestimmen und auf mögliche Korrelationen mit metabolischen Parametern sowie einer subklinischen Atherosklerose hin zu untersuchen.
Patienten und Methoden
In die Studie aufgenommen wurden 34 NAFLD-Patienten und 35 gesunden Probanden. NAFLD-Patienten hatten erhöhte Leberenzyme und eine sonographisch graduierte Steatosis hepatis, die Probanden normwertige Leberenzyme und keine sonographisch nachzuweisende Steatosis. H-FABP wurde mit einer ELISA(„enzyme-linked immunosorbent assay“)-Methode ermittelt und auf mögliche Korrelationen mit metabolischen Parametern sowie subklinischer Atherosklerose untersucht. Über die sonographische Messung der Intimadicke der A. carotis („carotid artery intima media thickness“, CIMT) im hochauflösenden B-Modus wurde die subklinische Atherosklerose bestimmt.
Ergebnisse
H-FABP-Serumkonzentrationen waren bei NAFLD-Patienten im Vergleich mit gesunden Probanden erhöht (16,3±4,0 vs. 13,8±2,1 ng/ml; p<0,001). CIMT-Werte waren bei NAFLD-Patienten höher als bei den Kontrollen 0,64±0,17 vs. 0,43±0,14 mm, p=0,009). Signifikante positive Korrelationen bestanden zwischen H-FABP-Serumkonzentrationen und BMI (r=0,255, p=0,042), Nüchternglukosekonzentrationen (r=0,300, p=0,013), CIMT (r=0,335, p=0,043) und HOMAR-IR („homeostasis model assessment-estimated insulin resistance“, r=0,156, p=0,306). In der multiplen Regressionsanalyse bestand ein unabhängiger Zusammenhang nur zwischen H-FABP-Konzentrationen und CIMT (p=0,04).
Fazit
H-FABP-Serumkonzentrationen sind bei NAFLD-Patienten erhöht. Unsere Ergebnisse könnten darauf hinweisen, dass H-FABP bei diesen Patienten nicht nur ein Marker für subklinische Myokardschädigungen ist, sondern auch für eine subklinische Atherosklerose − unabhängig von einem metabolischen Syndrom und kardialen Risikofaktoren.

Similar content being viewed by others

Abbreviations
- NAFLD:
-
Nonalcoholic fatty liver disease
- NASH:
-
Nonalcoholic steatohepatitis
- CIMT:
-
Carotid artery intima–media thickness
- H-FABP:
-
Heart type fatty acid binding protein
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- GGT:
-
Gama glutamyl transferase
- BMI:
-
Body mass index
- HOMA-IR:
-
Homeostasis model assessment-estimated insulin resistance
- ELISA:
-
Enzyme linked immunosorbent assay
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- TnT:
-
Troponin-T
- NR:
-
Normal range
References
Angulo P (2002) Medical progress: nonalcoholic fatty liver disease. N Engl J Med 346:1221–1231
Edmison J, McCullough AJ (2007) Pathogenesis of nonalcoholic steatohepatitis: human data. Clin Liver Dis 11:75–104
Marchesini G, Brizi M, Bianchi G, Tomassetti S et al (2001) Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes 50:1844–1850
Polak JF, Pencina MJ, Pencina KM et al (2011) Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med 365:213–221
O’Leary DH, Polak JF, Kronmal RA et al (1999) Carotid artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med 340:14–22
Salonen JT, Salonen R (1993) Ultrasound B-mode imaging in observational studies of atherosclerotic progression. Circulation 87(suppl):II56–II65
Chambless LE, Heiss G, Folsom AR et al (1997) Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. Am J Epidemiol 146:483–494
Salonen R, Salonen JT (1990) Progression of carotid atherosclerosis and its determinants: a population-based ultrasonography study. Atherosclerosis 81:33–40
Fournier NC, Richard MA (1990) Role of fatty acid-binding protein in cardiac fatty acid oxidation. Mol Cell Biochem 98:149–159
Pelsers MM, Hermens WT, Glatz JF (2005) Fatty acid-binding proteins as plasma markers of tissue injury. Clin Chim Acta 352:15–35
Adams JE, Trent R, Rawles J (1993) Earliest electrocardiographic evidence of myocardial infarction: implications for thrombolytic treatment. Br Med J 307:409–413
Ishii J, Wang JH, Naruse H et al (1997) Serum concentrations of myoglobin vs. human heart-type cytoplasmic fatty acid-binding protein in early detection of acute myocardial infarction. Clin Chem 43:1372–1378
Kleine AH, Glatz JFC, Nieuwenhoven FA van et al (1992) Release of heart fatty acid-binding protein into plasma after acute myocardial infarction in man. Mol Cell Biochem 116:155–162
Vuilleumier N, Righini M, Perrier A et al (2008) Correlation between cardiac biomarkers and right ventricular enlargement on chest CT in non massive pulmonary embolism. Thromb Res 21:617–624
Sugiura T, Takase H, Toriyama T et al (2005) Circulating levels of myocardial proteins predict future deterioration of congestive heart failure. J Card Fail 11:504–509
Nagahara D, Nakata T, Hashimoto A et al (2006) Early positive biomarker in relation to myocardial necrosis and impaired fatty acid metabolism in patients presenting with acute chest pain at an emergency room. Circ J 70:419–425
Arimoto T, Takeishi Y, Niizeki T et al (2007) Cardiac sympathetic denervation and ongoing myocardial damage for prognosis in early stages of heart failure. J Card Fail 13:34–41
Niizeki T, Takeishi Y, Takabatake N et al (2007) Circulating levels of heart-type fatty acid-binding protein in a general Japanese population: effects of age, gender, and physiologic characteristics. Circ J 71:1452–1457
Komamura K, Sasaki T, Hanatani A et al (2006) Heart-type fatty acid binding protein is a novel prognostic marker in patients with non-ischaemic dilated cardiomyopathy. Heart 92:615–628
Wunderlich MT, Hanhoff T, Goertler M et al (2005) Release of brain-type and heart type fatty acid-binding proteins in serum after acute ischaemic stroke. J Neurol 252:718–724
Renaud B, Ngako A (2007) Heart-type fatty acid-binding proteins (H-FABP): a reliable tool for initial risk stratification of pulmonary embolism? Eur Heart J 28:146–157
Oktay B, Akbal E, Firat H et al (2008) Evaluation of the relationship between heart type fatty acid binding protein levels and the risk of cardiac damage in patients with obstructive sleep apnea syndrome. Sleep Breath 12:223–228
Zimmermann-Ivol CG, Burkhard PR, Le Floch-Rohr J et al (2004) Fatty acid binding protein as a serum marker for the early diagnosis of stroke: a pilot study. Mol Cell Proteomics 3:66–72
Wada-Isoe K, Imamura K, Kitamaya M et al (2008) Serum heart-fatty acid binding protein levels in patients with Lewy body disease. J Neurol Sci 266:20–24
Akbal E, Özbek M, Güneş F et al (2009) Serum heart type fatty acid binding protein levels in metabolic syndrome. Endocrine 36:433–437
Karbek B, Özbek M, Bozkurt NC et al (2011) Heart-type fatty acid binding protein (H-FABP): relationship with arterial intima-media thickness and role as diagnostic marker for atherosclerosis in patients with impaired glucose metabolism. Cardiovasc Diabetol 2:10–37
Hamaguchi M, Kojima T, Itoh Y et al (2007) The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol 12:2708–2715
Bhatia LS, Curzen NP, Calder PC et al (2012) Non-alcoholic fatty liver disease: a new and important cardiovascular risk factor? Eur Heart J 33:1190–2000
Fraser A, Harris R, Sattar N et al (2007) Gamma-glutamyltransferase is associated with incident vascular events independently of alcohol intake: analysis of the British Women’s Heart and Health Study and Meta-Analysis. Arterioscler Thromb Vasc Biol 27:2729–2735
Mottillo S, Filion KB, Genest J et al (2010) The metabolic syndrome and cardiovascular risk: a systematic review and meta-analysis. J Am Coll Cardiol 56:1113–1132
Lucero D, Zago V, Lopez GI et al (2011) Pro-inflammatory and atherogenic circulating factors in nonalcoholic fatty liver disease associated to metabolic syndrome. Clin Chim Acta 412:143–147
Wong CKL, Burgess MI, Pugh CJ et al (2011) Elevated liver fat in non alcoholic fatty liver disease is associated with impaired myocardial relaxation. J Diabetes 3:202
Wong CK, Burgess MI, Irwin A et al (2010) Evidence of diastolic dysfunction in NAFLD: a study using tissue Doppler echocardiography. Diabetologia 53:495–496
Seo JM, Park TH, Lee DY et al (2011) Subclinical myocardial dysfunction in metabolic syndrome patients without hypertension. J Cardiovasc Ultrasound 19:134–139
Dinh W, Lankisch M, Nickl W et al (2011) Metabolic syndrome with or without diabetes contributes to left ventricular diastolic dysfunction. Acta Cardiol 66:167–174
Witteles RM, Fowler MB (2008) Insulin-resistant cardiomyopathy clinical evidence, mechanisms, and treatment options. J Am Coll Cardiol 51:93–102
Tanaka T, Hirota Y, Sohmiya K et al (1991) Nishimura S, Kawamura K. Serum and urinary human heart fatty acid-binding protein in acute myocardial infarction. Clin Biochem 24:195–201
Glatz JF, Kleine AH, Nieuwenhoven FA van et al (1994) Fatty acid-binding protein as a plasma marker for the estimation of myocardial infarct size in humans. Br Heart J 71:135–140
Setsuta K, Seino Y, Ogawa T et al (2002) Use of cytosolic and myofibril markers in the detection of ongoing myocardial damage in patients with chronic heart failure. Am J Med 113:717–722
Arimoto T, Takeishi Y, Shiga R et al (2005) Prognostic value of elevated circulating heart-type fatty acid binding protein in patients with congestive heart failure. J Card Fail 11:56–60
Niizeki T, Takeishi Y, Arimoto T et al (2005) Risk stratification using a combination of heart-type fatty acid binding protein and brain natriuretic peptide in patients hospitalized for congestive heart failure. Circ J 69:922–927
Niizeki T, Takeishi Y, Arimoto T et al (2005). Serum heart-type fatty acid binding protein predicts cardiac events in elderly patients with chronic heart failure. J Cardiol 46:9–15
Niizeki T, Takeishi Y, Arimoto T et al (2007) Heart-type fatty acid-binding protein is more sensitive than troponin T to detect the ongoing myocardial damage in chronic heart failure patients. J Card Fail 13:120–127
Ohno K, Tsutamoto T, Ishikawa C et al (2004) Relationship between the transcardiac increase of plasma heart-type fatty acid-binding protein and left ventricular remodeling in patients with dilated cardiomyopathy J Am Coll Cardiol 3:1031–1134
Morioka N, Shigematsu Y, Hamada M et al (2005) Circulating levels of heart-type fatty acid-binding protein and its relation to thallium-201 perfusion defects in patients with hypertrophic cardiomyopathy. Am J Cardiol 195:1334–1337
Lim TK, Lim E, Dwivedi G et al (2008) Normal value of carotid intima-media thickness—a surrogate marker of atherosclerosis: quantitative assessment by B-mode carotid ultrasound. J Am Soc Echocardiogr 21:112–116
Raitakari OT, Juonala M, Kähönen M et al (2003) Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA 290:2277–2283
Tzou WS, Douglas PS, Srinivasan SR et al (2005) Increased subclinical atherosclerosis in young adults with metabolic syndrome: the Bogalusa Heart Study. J Am Coll Cardiol 46:457–463
Skilton MR, Moulin P, Serusclat A et al (2007) A comparison of the NCEPATP III, IDF and AHA/NHLBI metabolic syndrome definitions with relation to early carotid atherosclerosis in subjects with hypercholesterolemia or at risk of CVD: evidence for sex-specific differences. Atherosclerosis 190:416–422
Czernichow S, Bertrais S, Blacher J et al (2005) Metabolic syndrome in relation to structure and function of large arteries: a predominant effect of blood pressure. A report from the SU.VI.MAX. Vascular Study. Am J Hypertens 18:1154–1160
Bertoni AG, Wong ND, Shea S et al (2007) Insulin resistance, metabolic syndrome, and subclinical atherosclerosis: the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 30:2951–2956
Marchesini G, Bugianesi E, Forlani G et al (2003) Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 37:917–923
Rector RS, Thyfault JP, Wei Y et al (2008) Non-alcoholic fatty liver disease and the metabolic syndrome: an update. World J Gastroenterol 14:185–192
Kim JH, Kim SY, Jung ES et al (2011) Carotid intima-media thickness is increased not only in non-alcoholic fatty liver disease patients but also in alcoholic Fatty liver patients. Digestion 84:149–155
Wong VW, Wong GL, Yip GW et al (2011) Coronary artery disease and cardiovascular outcomes in patients with nonalcoholic fatty liver disease. Gut 60:1721–1727
Sun L, Lu SZ (2011) Association between nonalcoholic fatty liver disease and coronary artery disease severity. Chin Med J (Engl) 124:867–872
Mohammadi A, Bazazi A, Ghasemi-Rad M et al (2011) Evaluation of atherosclerotic findings in patients with nonalcoholic fatty liver disease. Int J Gen Med 4:717–722
Kim D, Choi SY, Park EH et al (2012) Nonalcoholic fatty liver disease is associated with coronary artery calcification. Hepatology 56:605–613
Kang MK, Yoon H, Seon H et al (2011) Association between nonalcoholic fatty liver disease and subclinical coronary atherosclerosis determined by MDCT. Hepatology 54:1115A–1116A
Conflict of interest
On behalf of all authors, the corresponding author states that there are no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Financial support
No financial support was received for the study.
Ethics adherence
The study was approved by the ethics review committee of our hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Başar, Ö., Akbal, E., Köklü, S. et al. Increased H-FABP concentrations in nonalcoholic fatty liver disease. Herz 38, 417–422 (2013). https://doi.org/10.1007/s00059-012-3714-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-012-3714-x
Keywords
- Nonalcoholic fatty liver disease
- H-FABP
- Subclinical myocardial damage
- Subclinical atherosclerosis
- Carotid intima–media thickness