Summary
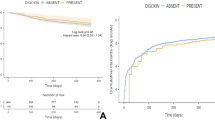
Digoxin therapy has been suggested to increase mortality risk in survivors of acute myocardial infarction. Since digoxin is a drug with a narrow therapeutic/toxic ratio, we raised the hypothesis that the association between digoxin and post myocardial infarction mortality may have a dose-dependent relationship. The purpose of this study was to evaluate this hypothesis. We retrospectively analyzed data from 1731 survivors of acute myocardial infarction. At the time of hospital discharge, 175 patients (10%) were taking digoxin. The exact dosage of digoxin was ascertained in 153 (87%) patients. Patients were divided into two groups based on the weekly dosage of digoxin at hospital discharge: The first group included 41 patients who were treated with a low dose (≤1.5 mg per week, usually 0.125 mg daily). The second group included 112 patients treated with a full dose (>1.5 mg per week, usually 0.25 mg daily). Both groups were comparable with regard to mean age, gender, history of prior myocardial infarction, diabetes mellitus, hypertension, and prior angina. There were no significant differences in the incidence of inhospital complications, such as heart failure, atrial fibrillation, ventricular tachycardia, ventricular fibrillation, and postinfarction angina. One year mortality was significantly higher among patients treated with a full dose [19 of 112 (17%)] than patients treated with a low dose of digoxin [1 of 41 (2%); p< 0.02] Multivariate analysis performed by the Cox proportional hazards model identified treatment with a full dose of digoxin as an independent determinant associated with increased death during the first year after myocardial infarction (hazard ratio 10.7; 95% confidence interval 1.4–80.5). Thus, mortality among myocardial infarction survivors treated with digoxin was related to a full-dose therapy. Patients treated with a low dose experienced a low mortality rate. Our findings raise concern that digoxin may exert a dose-dependent deleterious effect upon the survival of patients recovering from acute myocardial infarction.
Similar content being viewed by others
References
Yusuf S, Wittes J, Bailey K, Furberg C. Digoxin—a new controversy regarding an old drug: The pitfalls of inappropriate methods.Circulation 1986;73:14–18.
Fleiss JL, Bigger T, Rolnitzky LM, Is catch 22 alive and well and living at NHLBI? Reactions to ‘Digitalis—a new controversy regarding an old drug.”Circulation 1986;73:19–20.
Yusuf S, Garg R, Held P, Gorlin R. Need for a large randomized trial to evaluate the effects of digitalis on morbidity and mortality in congestive heart failure.Am J Cardiol 1992;69:64G-70G.
Marcus FI. Digitalis is effective, but is it safe?Cardiovasc Drugs Ther 1993;7:893–896.
Maroko PR, Kjekshus JK, Sobel BE, et al. Factors influencing infarct size following experimental coronary artery occlusions.Circulation 1971;43:67–82.
Lynch JJ, Lucchesi BR. Effect of digitalis on the extent of injury and the severity of arrhythmias during acute myocardial ischemia and infarction in the dog.J Cardiovasc Pharmacol 1988;11:193–203.
Moss AJ, Davis HT, Conard DL, DeCamilla JJ, Odoroff CL. Digitalis-associated cardiac mortality after myocardial infarction.Circulation 1981;64:1150–1155.
Bigger AJ, Fleiss JL, Rolnitzky LA, Merab JP, Ferrick KJ. Effect of digitalis treatment on survival after acute myocardial infarction.Am J Cardiol 1985;55:623–630.
The Digitalis Subcommittee of the Multicenter Post-Infarction Research Group. The mortality risk associated with digitalis treatment after myocardial infarction.Cardiovasc Drugs Ther 1987;1:125–132.
Akiyama T, Pawitan Y, Campbell WB, et al. Effects of advancing age on the efficacy and side effects of antiarrhythmic drugs in post-myocardial infarction patients with ventricular arrhythmias. The CAST Investigators.J Am Geriatr Soc 1992;40:666–672.
Sweeney MO, Moss AJ, Eberly S. Instantaneous cardiac death in the post hospital period after acute myocardial infarction.Am J Cardiol 1992;70:1375–1379.
Leor J, Goldbourt U, Behar S, Kaplinski E, Rabinovitz B. Is it safe to prescribe digoxin to patients recovered from myocardial infarction? Observations in patients at low and intermediate risk.Cardiovasc Drugs Ther 1995;9:65–73.
Ryan TJ, Baiely KR, McCable CH, et al. The effects of digitalis on survival in high-risk patients with coronary artery disease.Circulation 1983;67:735–742.
Byington R, Goldstein S, for the BHAT Research Study Group. Association of digitalis therapy with mortality in survivors of acute myocardial infarction: Observations in the Beta-Blocker Heart Attack Trial.J Am Coll Cardiol 1985;6:976–982.
Madsen EB, Glipin E, Henning H, et al. Prognostic importance of digitalis after myocardial infarction.J Am Coll Cardiol 1984;3:681–689.
Muller JE, Turi ZG, Stone PH, et al. Digitalis therapy and mortality after myocardial infarction. Experience in the MILIS study.N Engl J Med 1986;314:265–271.
The Israeli Study Group: Secondary Prevention Reinfarction Israeli Nifedipine Trial (SPRINT): A randomized intervention trial of nifedipine in patients with acute myocardial infarction.Eur Heart J 1988;9:354–364.
Blackburn H. Electrocardiographic classification for population comparisons: The Minnesota code.J Electrocardiol 1969;2:5–9.
Killip T, Kimbal JT. Treatment of myocardial infarction in a coronary care unit: A two year experience with 250 patients.Am J Cardiol 1967;20:457–464.
SAS Institute Inc. SAS technical report P-229.SAS/STAT Software: Changes and Enhancements, Release 6.07. Cary, NC: SAS Institute, 620 pp.
Mancini DM, Benotti JR, Elkayam U, et al. Antiarrhythmic drug use and serum levels of digitalis are independent adverse prognostic factors in patients with chronic heart failure (abstr.)Circulation 1991;84:II243.
Ferguson DW, Berg WJ, Sanders JS, Roach PJ, Kempf JS, Kienzel MG. Sympathoinhibitory responses to digitalis glycosides in heart failure patients.Circulation 1989;80:65–77.
Gheorghiade M, Ferguson D. Digoxin: A neurohormonal modulator in heart failure.Circulation 1991;84:2181–2186.
Feldman AM, Bristow MR, Parmley WW, et al. Effects of vesnarinone on morbidity and mortality in patients with heart failure.N Engl J Med 1993;329:149–155.
Nowak R. Problems in clinical trials go far beyond misconduct.Science 1994;264:1538–1541.
Author information
Authors and Affiliations
Consortia
Additional information
See Appendix.
Rights and permissions
About this article
Cite this article
Leor, J., Goldbourt, U., Rabinowitz, B. et al. Digoxin and increased mortality among patients recovering from acute myocardial infarction: Importance of digoxin dose. Cardiovasc Drug Ther 9, 723–729 (1995). https://doi.org/10.1007/BF00878556
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00878556